1. INTRODUCTION
Leishmaniasis, a parasitic disease caused by the protozoan parasites of the genus Leishmania, is transmitted by phlebotomine sandflies and has been detected in many countries worldwide (Adebayo and Suleman, 2013). Cutaneous leishmaniasis (CL) is the most common form; around 95% of cases occur in the Middle East, Central Asia, the Americas, and the Mediterranean basin; about 200,000 new cases occur worldwide yearly reported to the World Health Organization (WHO); this form causes skin lesions, mostly ulcers, on exposed parts of the body; these can then leave the patient with persisting scarring, causing significant stigma or disability (WHO, 2023). The number of leishmaniasis cases continues to climb, and the medication used for treating it is often toxic, though not usually efficient, and has an effect either directly or indirectly on health economics. As a result, global nature is focused on developing a novel remedy (De Paula et al., 2019). Morocco, a Mediterranean country in North Africa and an endemic region, reported 49,003 cases of CL between 2012 and 2022 (WHO, 2023).
Morocco’s botanical and ecological diversity is characterized by a rich flora and fauna population, which makes the region’s ecosystems unique (Guennoun et al., 2024). The conservation of botanical diversity is particularly important for the ecological integrity of Morocco as a whole, given contemporary threats such as habitat destruction and climate change. It is therefore important to protect endemic medicinal plants not only for cultural heritage but also to ensure the continuation of the supply of natural products that are important for human health (Squalli et al., 2024).
In addition to its great botanical and ecological diversity, several ethnobotanical surveys have highlighted the widespread use of medicinal plants in Morocco and revealed the importance of medicinal plant utilization through quantitative studies (Barkaoui et al., 2017; Bouyahya et al., 2017; Eddouks et al., 2017). In addressing the country’s leishmaniasis epidemic and combating drug resistance, it is critical to screen for alternative therapeutic compounds from medicinal plants. Moreover, the search for natural anti-leishmanial compounds in Morocco remains a relatively recent and emerging field of research (Abdlaali et al., 2020). On the other side, macrophages exposed to Leishmania generate reactive nitrogen species and reactive oxygen species (ROS), that aid in the regulation of the inflammatory reaction controlled through the cellular antioxidant defense system (Alkathiri et al., 2017).
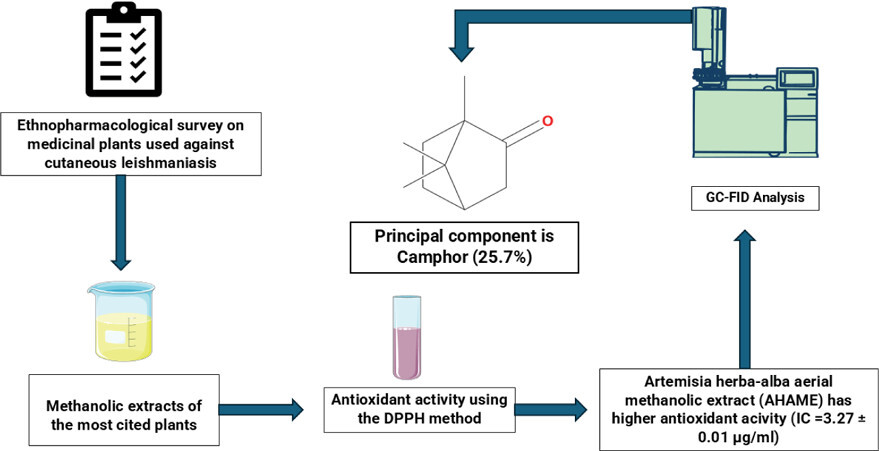
In Morocco, few studies have reported using medicinal plants to treat CL. Therefore, the present study aims to understand health professionals’ knowledge regarding the use of medicinal plants by local communities in the Marrakech–Safi region of Morocco to treat CL and evaluate their antioxidant activity.
2. METHODS
2.1. Study Area
The Marrakech–Safi region, located in central Morocco, spans an area of 41,404 km2, representing 6% of the national territory. It comprises one prefecture Marrakech and seven provinces: Chichaoua, El Haouz, El Kelaa des Saraghna, Rahamna, Essaouira, Safi, and Youssoufia (MEW, 2021). The region is characterized by a highly contrasting climate, ranging from dry plains to cold and humid mountain areas. It has three main weather stations located in Marrakech, Essaouira, and Safi. Average annual temperatures vary from 20.4°C in Marrakech to 17.8°C in Essaouira, with Safi’s weather station averaging 18.6°C. Additionally, the average yearly relative humidity ranges from 57% in Marrakech to 81% in Essaouira. Rainfall generally varies between 200 and 400 mm/year, reaching up to 800 mm/year in Safi and 800–1000 mm/year in the high El Haouz mountains (METSD, n.d.).
2.2. Data Collection
This study was carried out between April and November 2023 among all health professionals working in public health institutions across the Marrakech–Safi region in central Morocco, where several leishmaniases outbreaks have recently been declared (Amane et al., 2022). Data were collected through a self-administered questionnaire created in Google Forms, containing open-ended, direct, and semi-direct questions. This quantitative tool was designed to collect information on the socio-professional characteristics of participants. Besides, knowledge gathered by ethnopharmacological survey with health workers including (a) ethnomedicinal properties (local name, parts of plants, and the way of preparation) of plants and (b) health professionals´ opinions about using medicinal plants by the population and any prior experience with CL patient; and before implementing this ethnopharmacological survey, it was examined and verified with 30 health professionals from the Marrakech–Safi region, achieving a Cronbach’s alfa of 0.798), with acceptable internal consistency (Umaji and Paireekreng, 2023).
2.3. Plant Material
Leaves and aerial parts of selected plants were collected from different places in the Marrakech–Safi region, M. vulgare (latitude 32° 19’ 29”N, longitude 9° 10’ 34”W), A. herba alba (latitude 31° 31’ 20” N, longitude 9° 26’ 9”W), and O. basilicum L. (latitude 32° 24’ 53” N, longitude 9° 1’ 12” W), from January 2024 to April 2024. The samples were dried at 40 °C in the oven for 48 hours. Voucher samples were identified and deposited in the Laboratory of Water Sciences, Microbial Biotechnologies, and Natural Resources Sustainability (AQUABIOTECH), Faculty of Sciences-Semlalia, University Cadi Ayyad, Marrakech, Morocco. M. vulgare (A111), A. herba alba (A112), and O. basilicum L. (A113).
2.4. Antioxidant Activity
30 grams of the dried leaves of M. vulgare L. and O. basilicum L., and the aerial part of A. herba alba were powdered and extracted by the percolation method using ⩾99.8% methanol for 24 h. The extract was then filtered by filter paper and concentrated under vacuum conditions at 46°C using a rotary evaporator and kept at –20°C until testing.
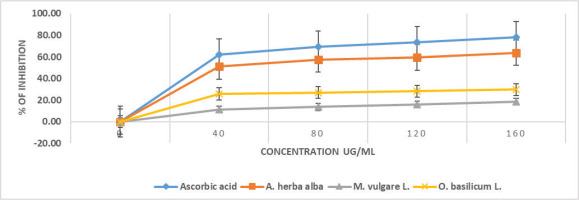
To evaluate the antioxidant activity of the extract, we used the 2,2-diphenyl-1-picrylhydrazyl radical (DPPH) assay. In this essay, 0.75 mL of a methanolic DPPH solution was mixed with 0.2 mL of the methanolic extract at varying concentrations (40, 80, 120, and 160 g/mL). The mixture was then shielded from light at room temperature for 30 min. Following this incubation, the absorbance was recorded at 517 nm, using a negative control of 0.75 mL of the DPPH solution and 0.2 mL of methanol. The study also included positive controls, such as ascorbic acid. The percentage of inhibition was calculated using the formulas:
Free-radical scavenging activity (%) = AA − AB / AA × 100
AA: The absorbance value in the DPPH solution that does not contain the extract.
AB: The absorbance value in the DPPH solution containing the extract.
2.5. GC-FID Analysis
The chemical composition of the Artemisia herba-alba aerial methanolic extract (AHAME) was analyzed using GC-FID. A capillary column (30 m length × 0.25 mm internal diameter × 0.25 μm film thickness), (95% polydimethyl, 5% polydiphenylsiloxane) was used for the GC analysis. After 1 minute, the oven’s temperature was raised to 230 °C at a pace of 3 °C per minute. 250 °C is the temperature of the injector and detector. The carrier gas, which had a steady flow rate of 1.5 mL/min, was helium 5.0. A 0.1 µl sample of A. herba alba methanolic extracts was injected at a 1:60 split ratio.
2.6. Data Analysis
Descriptive statistical methods using Jasp software 0.17.1.0 were applied to analyze and summarize the ethnomedicinal data, including the percentage distribution of plant families, species, preparation methods, and plant parts used. Also, the differences between means were determined using the least significant difference test at P < 0.05.
Checkmarket by Medalia was used to calculate the sample size with a 95% confidence level and a 5% margin of error, based on health reports (MHSP, 2022). Consequently, 364 participants were identified as the minimal required sample size. Given an estimated response rate of 50%, this number was doubled to account for non-participation, resulting in a target of 728 health professionals for the study (Amane et al., 2022).
3. RESULTS
Leishmaniasis is a serious public health concern in Morocco, and it has been declared a notifiable disease since 1995 (El-Mouhdi et al., 2020). In this study, 516 health workers agreed to participate from 728 contacted, of which 66.67% were female. The health workers interviewed were between 20 and 29 years old, while 21.13% of the health workers fell into the 30–39 years old age category. Nonetheless, 70.73% of health professionals have experience of up to 5 years, while only 14.73% have experience of 6–10 years. Furthermore, more than half of the participants (76.16%) are working in urban areas, with a predominance of Marrakech and Safi provinces (32.36% for each). Table 1 describes the sociodemographic characteristics of the health professionals in the study; 56.59 % of them confirmed that people use medicinal plants to treat CL; Furthermore, most respondents (36.01%) think that people use medicinal plants because they believe that traditional medicine is more effective; However, other health workers declared that the cause referred to the health centers offering treatment are far away or people prefer traditional medicine with a percentage of 24.92% and 27.97%, respectively (Table 2).
Table 1
Sociodemographic, educational, and professionalcharacteristics of the study participants (n = 516).
Table 2
Some questions referred to cutaneous leishmaniasis and medicinal plants.
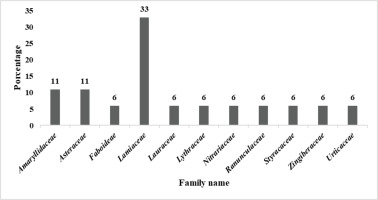
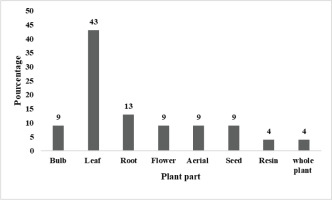
This survey collected ethnomedicinal information about 18 plant species recorded by informants for their medicinal benefits. The recorded species were distributed among 11 plant families. Lamiaceae represented 33% of the species, followed by Asteraceae (Rai and Lalramnghinglova, 2010) and Amaryllidaceae (11% each) (Figure 1). Besides, O. basilicum L, A. herba-alba, M. vulgare, A. cepa, A. sativum, and R. officinalis L are the most commonly used species in traditional medicine in the Marrakech–Safi region. All the medicinal plants were reported in their local names, listed in Table 3. In this research, the leaves are the most used plant parts (43%), followed by Roots (13%), and 9% for each part, aerial, bulbs, flowers, and seeds, while the other plant parts (resin and whole plant) do not exceed 5% for each (Figure 2). The principal modes of preparation were cataplasm (52%) and decoction (48%). In our study, AHAME shows a high antioxidant activity (Younsi et al., 2016), followed by O. basilicum L. (Figure 3) with an IC50 value of 3.27 ± 0.01 and 7.52 ± 0.02 μg/mL, respectively (Table 4).
Table 3
Inventory of plants used for cutaneous administration in treating cutaneous leishmaniasis in the Marrakech–Safi region.
Table 4
IC50 value of the antioxidant activity of selected methanolic extract plants.
The GC-FID analysis of AHAME identified eight major volatile compounds, presented in Table 5. Camphor (25.7%), caryophyllene oxide (19.1%), and caryophyllene (16.5%) were the three dominant constituents, collectively comprising over 60% of the total detected volatiles. The identified compounds were mainly classified into monoterpenes and monoterpenoids (α-thujene, camphor, β-thujone, and borneol) and sesquiterpenes and sesquiterpenoids (caryophyllene, germacrene D, spathulenol, and caryophyllene oxide). These include both hydrocarbon-based and oxygenated derivatives, such as ketones (camphor, β-thujone), alcohols (borneol, spathulenol), and epoxides (caryophyllene oxide). Notably, α-thujene (6.2%) was also detected as a minor monoterpene hydrocarbon. The chemical profile reveals a high proportion of oxygenated compounds and sesquiterpenoids, which is in agreement with previously reported data on A. herba-alba extracts from the North African region.
Table 5
GC-FID analysis of AHAME from Morocco: identified volatile compounds, their retention times, concentrations, and chemical classes.
| Peak# | Rt (min) | Area | Estimated concentration (%) | Probable compound | Chemical class | References |
|---|---|---|---|---|---|---|
| 1 | 11.919 | 147,998 | 6.2 | α-Thujene | Monoterpene | (Amara et al., 2025; Adams, 2007) |
| 2 | 13.554 | 610,548 | 25.7 | Camphor | Monoterpenoid | (Diass et al., 2022; Adams, 2007) |
| 3 | 53.556 | 193,445 | 8.1 | β-Thujone | Monoterpenoid | (Amara et al., 2025; Adams, 2007) |
| 4 | 54.030 | 393,234 | 16.5 | Caryophyllene | Sesquiterpene | (Basel, 2022; Adams, 2007) |
| 5 | 54.692 | 285,611 | 12.0 | Germacrene D | Sesquiterpene | (Diass et al., 2022; Adams, 2007) |
| 6 | 55.098 | 70,459 | 3.0 | Borneol | Monoterpene | (Amara et al., 2025; Adams, 2007) |
| 7 | 56.016 | 222,352 | 9.3 | Spathulenol | Sesquiterpenoid | (Basel, 2022; Adams, 2007) |
| 8 | 56.924 | 454,419 | 19.1 | Caryophyllene oxide | Sesquiterpenoid | (Basel, 2022; Adams, 2007) |
4. DISCUSSION
The objective of the present study, conducted in central Morocco, was to identify plants used by the population to treat CL (also known as “locally named by Tasmi Izi, Chniwla, Namousa, Chmaniaose, Hbouba”). This ethnopharmacological survey of health professionals’ knowledge of community use was conducted in the Marrakech–Safi region. In light of that, traditional herbal medicine continues to be an important topic for scientific research, especially when the literature and fieldwork data are properly evaluated. To address the epidemic of leishmaniasis in Morocco and combat drug resistance, it is crucial to screen for alternative molecules (Balahbib et al, 2020), based on traditional herbal uses, such evaluation findings can identify several plants that should be prioritized for further research into specific biological activity (Ali et al., 2004).
Firstly, the identified species were divided among 11 plant families, Lamiaceae is an endemic family; (Tahraoui et al., 2007) and is the most used family against CL in the Marrakech–Safi region, representing 33% of the plant species. In addition, most species of this family contain active compounds like Iridoids, flavonoids, phenol acid derivatives, and diterpenes (Di Giorgio et al., 2008). Also, many Lamiaceae plants are utilized to treat CL in the Tafilalt region (El Rhaffari and Zaid, 2002). The richness of Moroccan flora makes this family the most commonly used, and it has been the most reported family in several ethnopharmacological studies in other Moroccan regions. (Bourhia et al., 2019; Eddouks et al., 2017; Salhi et al., 2019; Tahraoui et al., 2007).
Secondly, the Asteraceae and Amaryllidaceae represent (11%) of each one. The Asteraceae family was traditionally used in traditional medicine to treat skin diseases, particularly CL (Amari et al., 2021; Salhi et al., 2019), are widely used in phytotherapy by the Tafilalt population (El Rhaffari and Zaid, 2002), Beyond the bounds, a study reported an antiprotozoal activity relationship of the Amaryllidaceae alkaloid compounds; however, certain findings suggest that the methylenedioxy group may have the potential to boost the antiprotozoal activity associated with these alkaloid compounds (Osorio et al., 2008).
In this research, the leaves are the most used plant parts (43%), These results are similar to those of previous studies (Barkaoui et al., 2017; Bourhia et al., 2019; Eddouks et al., 2017; El-Ghazouani et al., 2021; Salhi et al., 2019). These findings could be explained by the fact that leaves are the site of biochemical reactions involving photosynthesis. On the other hand, other ethnomedicinal surveys reported that leaves are the most used part to treat dermatological wounds and diseases (Grierson and Afolayan, 1999). Finally, the principal mode of preparation was cataplasm (52%) because it is the most commonly used preparation method to treat skin infections (Ennacerie et al., 2017), followed by decoction (48%) which is the most frequently used method by the population (Bourhia et al., 2019). On the other hand, six plants of the total reported medicinal plants are the most used against CL, O. basilicum L (24.77%), A. herba-alba (14.68%), M. vulgare (8.72%), A. cepa (6.88%), A. sativum (5.96%), and R. officinalis L (5.51%).
Firstly , O. basilicum L is a medicinally important herb from the Lamiaceae family (Khan et al., 2015) commonly known as basil and the local name is “Lhbaq” in the Safi-Marrakech region. Traditional Moroccan medicine often uses numerous plant species, including this plant, for curing infectious diseases; The phytochemical profile of O. basilicum indicates a rich presence of polyphenols, which have shown many biological activities including antimicrobial, antioxidant, and anti-inflammatory effects (Wójciak et al., 2024). Specifically, the essential oil has a significant effect against a variety of pathogens, suggesting its potential as a natural-based treatment against leishmaniasis and other infections widespread in the region (Kačániová et al., 2022).
This plant has a high use value in Agadir City, Morocco (El-Ghazouani et al., 2021). Besides, some studies worldwide reported that this plant has antileishmanial activity against Leishmania tropica (Khan et al., 2015), L. panamensis, L. braziliensis, L. major, and L. guyanensis. (Sanchez-Suarez et al., 2013). Moreover, to its medicinal properties, the ethnopharmacological use of O. basilicum in Central Morocco reflects a deep-rooted cultural practice where local populations rely on Indigenous plants for healthcare (Kačániová et al., 2022). The antimicrobial properties of basil are associated with its high concentration of compounds such as methyl chavicol and eugenol, which exhibit efficacy against a range of microorganisms (Santosh and Patil, 2021). Our results show that O. basilicum has a notable antioxidant activity with IC50 = 7.52 ± 0.02 μg/mL. This finding means that basil has been coupled with its ability to scavenge free radicals and protect against oxidative stress, additionally enhancing its allure as a natural remedy (Eid et al., 2023; Wójciak et al., 2024). Artemisia herba-alba, generally known as white wormwood, has drawn focus for its anti-leishmaniasis properties. This plant is traditionally used in Moroccan for a variety of health problems, including parasitic infections like leishmaniasis (Medjeldi et al., 2024).
Recently have demonstrated that extracts from A. herba-alba showed antileishmanial activity against L. infuntum (Aloui et al., 2016) and L. major, which are responsible for causing CL and VL; the bioactive compounds found in these extracts, like sesquiterpene lactones, contribute to their impact against these pathogens (Nasha’at and Al-Qushawi, 2014). Adding to that, a study reports that A. herba-alba was used to treat CL in Algeria (Amari et al., 2021); the locational proximity and environmental similarity to Morocco can explain this. In our study, this plant shows high antioxidant activity. This means that the plant’s antioxidants and also antimicrobial properties augment its therapeutic profile, making it a beneficial resource in traditional medicine (Wahnou et al., 2024). Besides, the ethnopharmacological value of this plant is reinforced by its incorporation into numerous herbal preparations conceived to treat infections and inflammatory conditions (Hafidh et al., 2022).
M. vulgare, widely known as white horehound, locally named “Merrout”, is commonly used in classical medicine in Bordj Bou Arreridj, Algeria (Adimi et al., 2023). This plant has been traditionally used to treat numerous diseases, including respiratory symptoms and skin diseases (Mssillou et al., 2022). Furthermore, M. vulgare proposes its efficiency as a natural therapeutic agent to combat this disease in Central Morocco (Adimi et al., 2023). Additionally, M. vulgare is frequently included in local herbal remedies, reflecting its importance and role in improving health outcomes through bio-based products in Morocco. (Laadim et al., 2017).
Continuing on this line, it exhibited the highest activity against Trypanosoma cruzi epimastigotes (Molina-Garza et al., 2014); Also it mentioned the antimicrobial properties of Trichomonas (Azimi Kohan et al., 2023); Considering this , M. vulgare can have the highest activity against the leishmania species spread in Morocco. On another note, R. officinalis L. is used as a medicinal plant in Sefrou city (center of Morocco) (Zeouk et al., 2020). Besides A. cepa being used against CL in Tafilalt city (El Rhaffari and Zaid, 2002), added to A. sativum and R. officinalis L showed potent leishmanicidal activity and could be utilized as an alternative medication to treat leishmaniasis (Sanchez-Suarez et al., 2013; Wabwoba et al., 2010).
In Morocco, R. officinalis L is tested against L. tropica, L. major, and L. infantum with the IC50 value of 3.5, 2.6, and 1.2 mg/mL, respectively (Bouyahya et al., 2017). However, the molecular characteristics of one region could be different from another one; for this reason, we can find a different result depending on the species of leishmania and their local foci.
Our GC-FID analysis of AHAME from central Morocco, which identified camphor, caryophyllene, caryophyllene oxide, and germacrene D as major constituents, shows both similarities and notable differences compared to previous studies on Moroccan A. herba-alba. Many earlier studies report camphor as a principal component, often in the range of 19–48% (Vernin et al., 1995), which aligns closely with our findings. For example, one GC-MS analysis found camphor at 26.02% (Baranová et al., 2025), and another reported 9.76% (Houti et al., 2023), confirming camphor’s consistent prominence but also highlighting regional and methodological variability. Other major compounds frequently reported include α- and β-thujone, 1,8-cineole, chrysanthenone, and chrysanthenyl acetate, with some chemotypes showing β-thujone as high as 23.2% and chrysanthenyl acetate up to 30% (Houti et al., 2023; Vernin et al., 1995). In contrast, our extract is distinguished by a higher proportion of caryophyllene and caryophyllene oxide, which are less dominant in many previous Moroccan samples, where sesquiterpenes like these are often present in lower concentrations or not highlighted as major constituents (Baranová et al., 2025; Vernin et al., 1995).
This variation may be attributed to differences in extraction methods (methanolic extract vs. hydrodistilled essential oil), plant chemotype, harvest time, and geography. Notably, your sample’s significant levels of caryophyllene and its oxide suggest a unique chemotype or extraction influence, as these compounds are recognized for their bioactivity but are not always abundant in essential oil studies from the region (Vernin et al., 1995). Overall, while our results confirm the expected dominance of camphor, they also reveal a distinct chemical fingerprint with elevated sesquiterpenes, setting our sample apart from the more common thujone and chrysanthenone-rich profiles previously described in Moroccan A. herba-alba (Baranová et al., 2025; Houti et al., 2023; Vernin et al., 1995).
To the best of our knowledge, there are no published studies in the provided search results specifically investigating the antileishmanial activity of camphor obtained from a methanolic extract. The available research focuses on the antileishmanial effects of methanolic extracts from various medicinal plants, Methanolic extracts are more likely to contain a broader range of polar and nonpolar compounds, and their activity is often attributed to this complex mixture rather than a single constituent like camphor; most antileishmanial studies involving camphor focus on essential oils not methanolic extract (Nosratabadi et al., 2015).
Camphor and its derivatives have demonstrated significant antileishmanial activity in both in vitro and in vivo studies; essential oils rich in camphor, such as those from Artemisia annua, exhibit potent leishmanicidal effects against both promastigote and intracellular amastigote forms of Leishmania donovani, with inhibitory concentrations (IC50) as low as 7.3 μg/mL for amastigotes comparable to some standard treatments (Islamuddin et al., 2014). Moreover, the mechanism involves induction of programmed cell death in the parasites, evidenced by externalization of phosphatidylserine, DNA fragmentation, dyskinetoplastidy, cell cycle arrest, loss of mitochondrial membrane potential, and generation of ROS; importantly, these camphor-rich oils showed no cytotoxicity to mammalian macrophages, even at high concentrations, and caused no detectable liver or kidney toxicity in treated animals, highlighting their safety profile (Islamuddin et al., 2014). In another study, a series of camphor hydrazone derivatives were synthesized and tested against Leishmania amazonensis; most compounds were active against the amastigote form, showing an IC50 of 21.78 µM close to the reference drug miltefosine, and all compounds were nontoxic to host macrophages at tested doses (da Silva et al., 2020). These findings suggest that camphor and its derivatives are promising candidates for the development of new, selective, and safe antileishmanial agents, though further research is needed to fully elucidate their mechanisms and optimize their therapeutic potential (da Silva et al., 2020; Islamuddin et al., 2014). In summary, to the best of our knowledge, there have been only a few studies on the anti-leishmanial potential in Morocco of O. basilicum L, A. herba-alba, and M. vulgare; however, there have been no studies on the antileishmanial activity of these plants in the Marrakech–Safi region (Central Morocco).
5. CONCLUSION
Our study highlights the most used medicinal plants for treating CL in the Marrakech–Safi region, with A. herba-alba emerging as a key species, widely used in traditional medicine, showing strong antioxidant activity, supported by the presence of camphor, a bioactive compound known for its antimicrobial and antiparasitic properties. The combination of antioxidants and antileishmanial effects suggests a dual mechanism that may help both inhibit the parasite leishmania and support tissue healing.
Given the limitations of current CL treatments, including cost, toxicity, and drug resistance, these findings support further investigation of traditional medicinal plants. Future research should focus on confirming these effects through in silico, in vitro, and in vivo studies while optimizing formulations for medical use. Harnessing such natural resources could offer safer, affordable, and locally accepted alternatives for managing this disease.