1. INTRODUCTION
Herbal remedies have been integral to traditional medicine for over 60,000 years (Al-Jaber et al., 2024). However, urbanization, migration, habitat loss, and lifestyle changes have led to a decline in ethnomedicinal knowledge, disrupting the intergenerational transfer of this vital information (Subramanyam et al., 2007; Teklehaymanot & Giday, 2007). The World Health Organization (WHO, 2013) launched the Traditional Medicine Strategy 2014–2023 in response to this growing concern. This strategy seeks to integrate ethnomedicinal, plant-based traditional medicine into mainstream healthcare. A key component of this initiative involves collecting reliable field-based data to support the exploration and documentation of medicinal plants (WHO, 2019).
Despite their significance, wetland plants have received comparatively less attention in ethnobotanical research than terrestrial plants, even in regions like India where they historically served as primary sources of food and traditional medicine (Sivaramanan & Sivapriya, 2024). From staple crops to cosmetics, wetland plant products are essential for human society. Wetlands, covering approximately 12.1 million km2, provide crucial ecosystem services, contributing an estimated 40.6% of the total universal value (Costanza et al., 2014; Ramsar Convention on Wetlands, 2018). WESs (Wetland ecosystem services) encompass goods and services from diverse water bodies, including marshes, swamps, bogs, and fens (Mitsch et al., 2015), that directly and indirectly enhance the quality of life (Millennium Ecosystem Assessment [MEA], 2005). Despite their recognized productivity, ecological importance, and the ratification of the Ramsar Convention by 169 countries, a 35% reduction in wetlands has been observed globally due to unsustainable exploitation since 1970 (Ghermandi et al., 2008; Mitsch & Gosselink, 2000; Rebelo et al., 2017). Wetlands are increasingly vulnerable due to the
expansion of human activities, including pollution, encroachment, harmful tourism, agricultural activities, urbanization, and overexploitation (Bassi et al., 2014).
India’s diverse topography and climatic conditions support a wide array of unique wetland habitats (Prasad et al., 2002). While estimates of the total wetland area in India vary considerably, ranging from 1 to 5% of the country’s geographical area, these wetlands harbor a significant portion, nearly one-fifth, of India’s known biodiversity (Space Applications Centre [SAC], 2011). In India, wetlands are indispensable for supporting diverse habitats and a rich variety of life. They also provide a wide range of ecological goods and services, offering numerous essential benefits to both ecosystems and human well-being (Bassi et al., 2014).
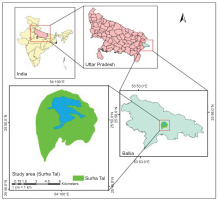
Wetlands, spanning diverse climatic zones and harboring different varieties of plant species, offer unique opportunities to investigate patterns of plant utilization across different regions. Local communities residing in or near these ecosystems often possess valuable traditional knowledge regarding the uses of wetland plants, particularly in the context of ethnomedicine. Documentation of this indigenous knowledge is not only crucial for conserving and sustainably managing medicinal plants but also opens avenues for the sustainable development of wetland-dependent communities. Surha Tal, a prominent freshwater lake in the Ballia district of Uttar Pradesh, India, undergoes significant expansion during the monsoon season, fostering rich biodiversity (Singh et al., 2017). The study focuses on wetlands and how local communities residing on the fringes of wetlands make use of medicinal plants found in that area.
The main objectives of the study are as follows:
To document the knowledge of ethnomedicinal plants prevalent in the local communities, including information on various parts of the plant, modes of application, and associated ailments.
To calculate quantitative indices based on ethnobotanical parameters such as Relative frequency citation, Use value, informant Consensus factor, and Fidelity level for the documented medicinal plants.
The research is primarily carried out to generate base data on the use of ethnomedicinal plants in the Surha Tal region, laying the groundwork for future pharmacological and phytochemical studies.
2. MATERIALS AND METHODS
2.1. Area of study and demographic details
Surha Tal, a natural lake located in the Ballia district of Uttar Pradesh, is the largest floodplain lake in the region (Figure 1). This oval-shaped, perennial meander of the Ganga River covers an area of 34.2 km2, with the lake itself occupying 26 km2. Situated at an altitude of 166 m, its coordinates are 25°48’N–25°52’N and 84°8’E–84°13’E. The wetland is officially designated as the “Jai Prakash Narayan Bird Sanctuary” (Srivastava & Srivastava, 2012).
The lake, approximately 17 km north of Ballia City, supports a diverse range of natural vegetation, including arable fields, macrophytes, and mesophytes. It is recognized for its significant avian biodiversity, particularly during the winter migratory season when it hosts an estimated 50,000 waterfowl. Surha Tal is classified as a high-priority wetland (Level V) due to its ecological and socioeconomic potential, despite limited data availability (Samant, 2000). Local communities utilize the lake’s resources for irrigation, livestock fodder, and domestic fuel. However, like many wetlands in densely populated areas, Surha Tal faces anthropogenic pressures such as uncontrolled fishing, water drainage for irrigation, weed infestation, and unsustainable resource exploitation.
Ballia district has the second-largest tribal population in Uttar Pradesh after Sonbhadra, based on the 2011 census. The Gonds and Kharwar are the predominant tribal communities, constituting 3.4% of the district’s total population of 3,239,774. The Gonds comprise over 75% of the tribal population, with 90.06% residing in rural areas. The Kharwar represents 16.87% of the tribal population, with 88.84% living in rural areas.
2.2. Collection of Ethnobotanical data
Data was collected through multiple field visits to the study area. Partially organized interviews were conducted along with questionnaire-based household surveys to gather information from local communities about their knowledge of the application of medicinal plants in treating various ailments. We designed a structured questionnaire for facilitating data collection, incorporating sections on informant consent, demographic details (name, age, gender), and specifics of medicinal plants (local names, usage, plant part used, preparation mode, and modes of utilization). Community participation was at free will, and consent was obtained from all informants. Comprehensive information on medicinal plants, encompassing local names, use value, modes of utilization, and plant parts used, was meticulously recorded. The survey process encouraged interactive knowledge exchange between researchers and informants, ensuring comprehensive documentation of local plant knowledge. Socioeconomic data, including age, gender, educational qualifications, and occupation, were also collected. Identification and collection of plant species were conducted with the assistance of key informants. Subsequently, plant identities were authenticated using relevant flora references, and scientific names were verified using The Plant List (www.theplantlist.org).
2.3. Data analysis
The data were collected, curated, and statistically analyzed with SPSS software. The preparation of the diagram was done using the circle package in R Studio.
2.3.1. Relative Frequency Citation
The relative frequency citation (RFC) was employed to assess the local importance of each plant species. This metric was calculated using the following formula:
Where FC is the number of informants mentioning the use of a particular species, and N is the total number of informants participating in the study. The RFC values range between 0 and 1, with higher values indicating greater local importance of the species. This method aligns with the approach used in previous ethnobotanical studies (Hoffman & Gallaher, 2007; Vitalini et al., 2013).
2.3.2. Use Value
The use value (UV) was computed to determine the relative importance of plant species based on the average number of uses mentioned by each informant. The formula used was:
Where Ui is the number of uses reported by each informant for a particular species, and N is the total number of informants (Phillips et al., 1994). A high UV signifies a plant with multiple reported uses, indicating its greater significance, whereas a low UV implies fewer reported uses.
2.3.3. Informant Consensus Factor
To evaluate the level of agreement among informants concerning the medicinal plants employed for various ailment categories, the Informant Consensus Factor (ICF) was calculated. Following the approach outlined in Heinrich et al. (1998), diseases were categorized into distinct groups. The ICF was then computed using the formula proposed by Trotter and Logan (1986).
Where Nur denotes the total number of use reports for a specific category, and Nt represents the total number of species utilized for that category. The ICF values range from zero to one, with higher values indicating greater agreement among informants.
2.3.4. Fidelity Level (%)
The percentage of fidelity level (FL%) was determined to identify the most preferred species for treating particular ailments (Hoffman & Gallaher, 2007). The following formula was used.
Where Np is the number of use reports mentioning a species for a specific ailment, and N is the total number of use reports for that species. A high FL value (approaching 100%) suggests that a plant is consistently used for a specific purpose, while a low FL value indicates its use for various ailments.
3. RESULTS
3.1. Demographic characteristics
Field surveys resulted in interviews with 96 informants, of whom 32 were traditional healers (Vaidyas & Daai), who served as key informants for this study. Male informants constituted the majority (65.62%), while female informants comprised 34.38% of the sample. The age distribution of informants spanned four groups: 20–35 years, 36–50 years, 51–65 years, and over 65 years. The largest proportion of participants (66.67%) fell within the age range of 35–65 years. Educational backgrounds varied among informants, with the largest group (40.62%) having completed secondary education. A small percentage (7.29%) reported being illiterate, who were predominantly over 65 years of age (Table 1).
Table 1
Demographic features of the indigenous informants in the study area.
3.2. Influences of sociodemographic variables
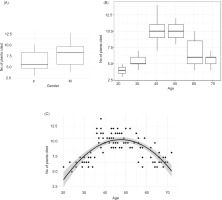
Our findings demonstrate a significant association between informant age and occupation, and the number of medicinal plants they identified. The awareness about the use of plants for herbal medicine preparation is more prominent in male informants (Figure 2A). Middle-aged traditional healers (36–65 years) exhibited a notably higher knowledge of medicinal plants compared to other age groups (Figure 2B). Regression analysis across different ethnic groups further corroborated the positive correlation between informant age and their knowledge of medicinal plants (Figure 2C). This suggests that experience and accumulated knowledge play a pivotal role in the identification and use of medicinal plants within these communities.
Figure 2
(A) Average number of medicinal plants reported by female and male informants. (B) Average number of medicinal plants reported by informants of different age groups. (C) Correlation between the indigenous informant’s awareness about medicinal plant citation and his or her age (R2 = 0.5252, p = 0, r = −0.0100663534).
3.3. Diversity and taxonomy of medicinal plants
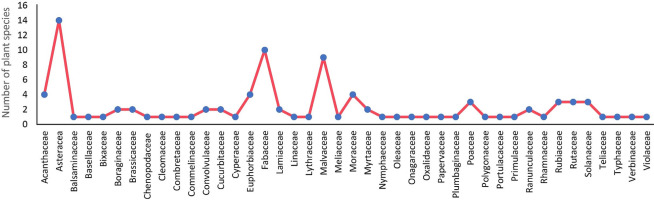
Ninety-six medicinal plants from 42 families were documented in this study and were utilized by local communities for treating various ailments. Asteraceae was the most represented family, with 14 species, followed by Fabaceae (10 species) and Malvaceae (9 species). Acanthaceae, Euphorbiaceae, and Moraceae contributed four species each. Families with three representatives included Poaceae, Rubiaceae, Rutaceae, and Solanaceae. Boraginaceae, Brassicaceae, Convolvulaceae, Cucurbitaceae, Lamiaceae, Myrtaceae, and Ranunculaceae were each represented by two species. The remaining 25 families were represented by a single species each (Figure 3).
3.4. Growth form of medicinal plants
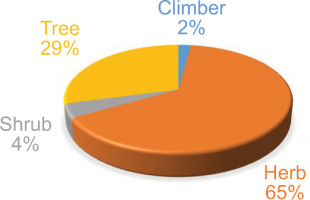
Various growth forms were identified, including herbs, shrubs, trees, and climbers. Herbs were the most used by local communities, with 62 species (65.00%) used for herbal medicine, followed by 28 species (29%) of trees, four species (4%) of shrubs, and two species (2.0%) of climbers (see Figure 4 and Table 2)
Table 2
Medicinal plants recorded with family, scientific name, habit, parts used, mode of use, UV (use value), and RF (relative frequency citation) and FL% (for diseases, i.e. bold written highlights in “Ailments” column)
3.5. Mode of preparation and administration of herbal medicine
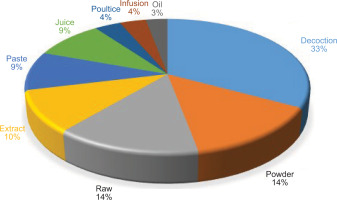
The most common method of formulation preparation or administration was decoction (33%), followed by powder and raw form (14% each), extract (10%), paste (9%), poultice (4%), and oil (3%) (as shown in Figure 5).
3.6. Frequency of plant parts used
Our findings reveal a diverse utilization of plant parts in traditional remedies, encompassing flowers, bark, rhizomes, grains, fruits, tubers, stems, seeds, leaves, roots, and whole plants. Leaves emerged as the most frequently used plant part, sourced from 54 species. This was followed by roots (23 species), whole plants (20 species), bark (18 species), flowers, fruits, and seeds (13 species each) (Figures 6A and 6B, and Table 2).
3.7. Informant consensus factor
Our analysis using the ICF revealed a high degree of agreement among participants regarding the medicinal plants used for various ailments (Figures 7A and 7B). To address the potential for a single plant treating multiple conditions, diseases were categorized into 16 ailment groups. ICF values, ranging from 0.75 to 0.94, demonstrated a substantial consensus among informants across these categories. Digestive diseases exhibited the highest ICF score (0.94), suggesting a strong agreement on plant remedies for this ailment. Conversely, gynecological issues, including menstrual disorders and leukorrhea, had the lowest ICF score (0.75), indicating a relatively lower level of consensus on treatments within this category.
Figure 7
(A) Informant consensus factor (ICF) of various ailment categories. (B) Chord diagram showing documented medicinal plants used in different ailment categories from the study area. BD: Blood diseases; CD: Connective diseases; CVD: Cardiovascular diseases; DD: Digestive diseases; EED: Ear and eye diseases; GD: Genitourinary diseases; GP: Gynecological problems; GS: General symptoms; ICF: Informant consensus factor; ID: Infectious diseases; IN: Injury; MD: Metabolic diseases; NP: Neoplasms; NSD: Nervous system disorder; Ntax: Total number of species used for a group of ailments; Nur: Total number of used reports for a group of ailments; PB: Poisonous bites; RD: Respiratory diseases; SD: Skin diseases.

3.8. Use value and relative frequency citation
The “use value,” which indicates importance, was calculated based on the frequency of reported medicinal applications. Aegle marmelos (L.) Corrêa emerged as the most preferred species (UV = 0.92), closely followed by Syzygium cumini (L.) Skeels (UV = 0.91). Other prominent species included Terminalia bellirica (Gaertn.) Roxb (UV = 0.87), Ricinus communis L. (UV = 0.86), Eclipta prostrata L., and Linum usitatissimum L. (both at UV = 0.85), and Chenopodium album L. (UV = 0.84). Conversely, Rungia repens L. Nees exhibited the lowest UV (0.08), suggesting minimal medicinal utilization in the region (Table 2).
Relative frequency of citation, an additional indicator of plant significance, corroborated the UV findings. The highest value was observed for Syzygium cumini (L.) Skeels (RFC = 0.62), Linum usitatissimum L. (RFC = 0.60), and Aegle marmelos (L.) Corrêa (RFC = 0.59) (Table 2). Species with higher reported uses (UV) were also more frequently cited (RFC) by informants for their medicinal benefits.
3.9. Fidelity level
This parameter assesses the relative importance of plants for specific ailment categories. Notably, Ricinus communis L. exhibited the highest FL (99.43%), primarily used for treating constipation . Syzygium cumini (L.) Skeels, with an FL of 99.09%, was predominantly employed for managing diabetes. Other species demonstrating high FL values included Aegle marmelos (L.) Corrêa (97.11%) for dysentery, Prosopis cineraria (L.) Druce (97.03%) for leprosy, and Linum usitatissimum L. (96%) for coronary heart disease and stroke (Table 2).
4. DISCUSSION
This study investigated the ethnomedicinal knowledge and practices associated with wetland areas of the Surha Tal region in India. The research documented 96 medicinal plant species and analyzed their use patterns, preparation methods, and cultural significance. Our findings underscore a concerning trend of declining traditional knowledge among younger generations, emphasizing the urgent need to preserve this invaluable cultural heritage. Additionally, we identified several key species exhibiting high UV and FL, highlighting their potential for further pharmacological investigation and conservation efforts.
The distribution of knowledge about medicinal plants was nonuniform among the communities. Consistent with previous studies (Geta et al., 2020; Khadim et al., 2024; Sharma et al., 2019; Tamene et al., 2024), older individuals (>35 years) in both Gond and Kharwar ethnic groups demonstrated a greater understanding compared to younger individuals (<35 years). This discrepancy may be attributed to the younger generation’s preference for allopathic medicine and reduced exposure to traditional practices. As Silva et al. (2011) suggest, older individuals have more opportunities for cultural and medicinal interactions with plants, reinforcing their knowledge base. The observed decline in ethnobotanical knowledge among the youth underscores the need for bridging this generational gap.
This erosion of traditional knowledge is further compounded by several factors, including a lack of interest among the youth, ineffective knowledge transmission methods (e.g. oral tradition, secrecy), and limited policy support for traditional medicine (Faruque et al., 2019). The migration of young healers to urban areas in seeking better economic prospects exacerbates this issue.
Gender is another test to determine the distribution of ethnobotanical knowledge across ethnic groups. In this study, the male informants were more knowledgeable about the use of medicinal plants for traditional remedies than females, which suggested a male-biased knowledge distribution (Asfaw et al., 2022; Faruque et al., 2019). Furthermore, it was observed that traditional knowledge about medicinal plants was not correlated with the level of formal education (Kutal et al., 2021; Silambarasan et al., 2023).
The wetland ecosystem, comprising both terrestrial and aquatic components, supports a rich diversity of plant life. This plant diversity not only underpins the region’s biodiversity but also serves as a vital resource for the healthcare and livelihoods of surrounding communities (Deka & Sarma, 2014). Asteraceae showed up as a highly represented family in the ethnomedicinal repertoire, consistent with findings from other regions (Bondya & Bharti, 2021; Khadim et al., 2024; Sõukand et al., 2022; Tamene et al., 2024). Along with Asteraceae, plant species of other families like Fabaceae, Malvaceae, Acanthaceae, Euphorbiaceae, Moraceae, and Poaceae were also frequently used to treat different diseases in the study area. The prevalence of these families may be attributed to their abundance and easy accessibility in the research area. The abundance and potential therapeutic properties of these plant families, including their aromatic compounds and diverse bioactive molecules, likely contribute to their widespread use (Bekele-Tesemma, 2007; Balick & Cox, 2020).
Herbs constituted the predominant life form among utilized medicinal plants, followed by trees. This preference aligns with previous reports (Agize et al., 2022; Bahadur et al., 2023; Tamene et al., 2024). The widespread availability, easy collection method, and potential cultural significance of herbs likely contribute to their prominence in traditional medicine.
The leaves were the most commonly used part by communities for medicinal purposes, which agreed with other ethnobotanical studies (Iyamah & Idu, 2015; Tamene et al., 2024). This preference may be due to the high concentration of bioactive compounds in leaves and their rapid regeneration capacity (Tugume & Nyakoojo, 2019).
We found decoction as a preferred herbal preparation, followed by powders and pastes. This aligns with the widespread use of decoctions in traditional medicine, potentially due to their efficacy in extracting plant constituents (Boadu & Asase, 2017; Agize et al., 2022; Ssenku et al., 2022; Tugume and Nyakoojo, 2019). Oral and topical routes were the primary modes of administration, consistent with previous observations (Bahadur et al., 2023; Khadim et al., 2024).
The high ICF values observed here suggest a strong reliance on local knowledge for healthcare within the community (Uddin & Hassan, 2014). The highest ICF for digestive diseases is consistent with other reports (Dery et al., 2023; Singh et al., 2012; Umair et al., 2017), possibly reflecting the reliability of indigenous people in traditional remedies. The second-highest ICF was observed for diabetes, a metabolic disorder likely due to socioeconomic reasons and lack of awareness (Muralidharan, 2024).
The RFC and UV provide insights into the cultural significance and perceived efficacy of specific plants. High RFC and UV values often correlate with species abundance and long-term use, suggesting their importance in the local ethnomedicinal system (Medeiros et al., 2012; Vitalini et al., 2013). The RFC and UV are consistent within a particular area, but can vary depending on the knowledge of indigenous people across different regions or even within the same region. Species consistently scoring high RFC and UV are prioritized for conservation and sustainable harvesting to prevent local extinction (Farooq et al., 2019; Kayani et al., 2014). Species exhibiting high RFC and UV, such as S. cumini, L. usitatissimum, and A. marmelos, warrant further investigation for various properties, potentially leading to novel drug discoveries (Amjad et al., 2020; Beshah et al., 2020; Mukherjee et al., 2012).
The FL highlights plants consistently used for specific ailments, indicating their potential as candidates for targeted pharmacological research (Amjad et al., 2020; Ralte et al., 2024). The plants with the highest FL values were R. communis L. (99.43%), S. cumini (L.) Skeels (99.09%), and A. marmelos (L.) Corrêa (97.11%). The high FL value for R. communis in treating constipation, despite its toxicity, underscores a requirement for careful evaluation and awareness of potential risks associated with traditional remedies (Marwat et al., 2017). In the present study, S. cumini (L.) Skeels are used to treat diabetes, cardiovascular, and spleen diseases, with the highest FL of 99.09% for diabetes. The peel, pulp, and seeds of the S. cumini (Jamun) are rich in antioxidants, polyphenols, flavonoids, minerals, vitamins, and other phytochemicals. A comprehensive analysis of Jamun’s nutritional and medicinal properties by Rizvi et al. (2022) reveals its positive effects on type 2 diabetes mellitus (T2DM), cardiovascular diseases, hypertension, hyperlipidemia, and obesity. Collectively, these benefits suggest that Jamun could play a protective role against metabolic syndrome.
5. CONCLUSION
The ethnobotanical survey of Surha Tal wetland offers significant insights into the traditional knowledge and practices of the local communities regarding the use of plants. This study underscores the deep-rooted relationship between indigenous people and their natural environment, highlighting how local flora plays a crucial role in healthcare, livelihood, and cultural practices. Many plants used in traditional medicine could serve as a basis for future pharmacological research and the discovery of potential compounds for making new drugs. In conclusion, this study not only helps document and validate the traditional use of plants but also opens doors for conservation efforts, scientific research, and community development initiatives, ensuring the sustainable use of the plant resources of Surha Tal wetland.
ACKNOWLEDGMENTS
The authors would like to extend their warmest thanks to the School of Environmental Sciences, Jawaharlal Nehru University, for their valuable administrative support.
AUTHOR CONTRIBUTIONS
Research concept and design, collection and/or assembly of data, data analysis, interpretation and the writing: A.K.O.; Collection and/or assembly of data: C.; assembly of data: K.P. All authors contributed to the critical revision, and the final draft was approved by all three authors.