1. INTRODUCTION
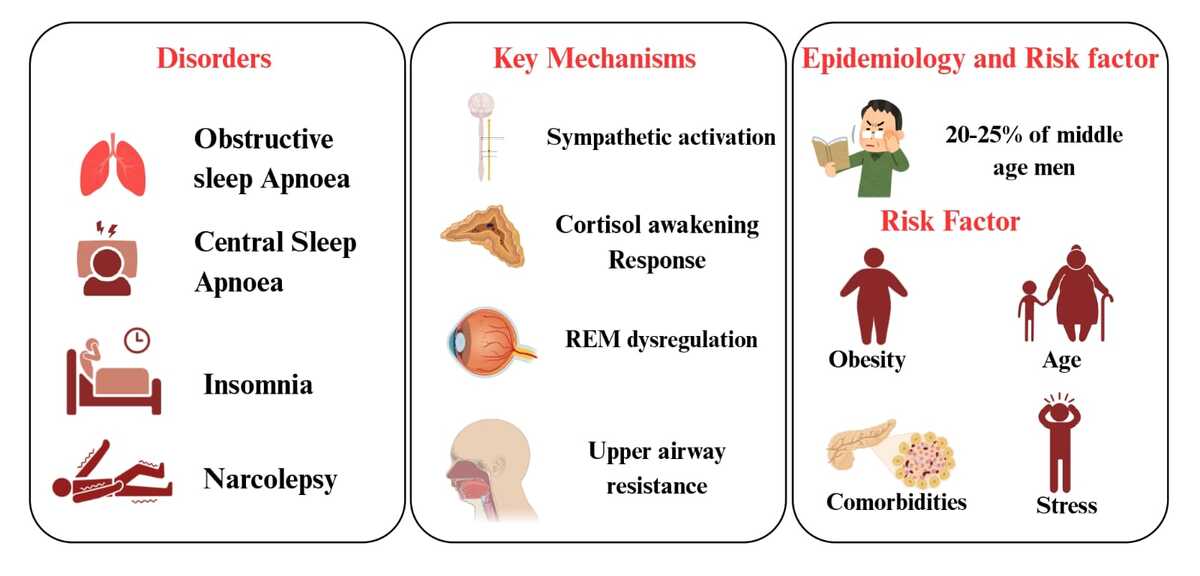
Sleep disorders are divided into seven main categories based on the International Classification of Sleep Disorders-3 (ICSD-3) diagnostic criteria: Circadian rhythm sleep-wake disorders, sleep-related movement disorders, central disorders of hypersomnolence, insomnia disorders, sleep-related breathing disorders (SBD), parasomnias, and other sleep disorders (L. Zhang et al., 2024) .Obstructive sleep apnoea (OSA) is without a doubt the most researched sleep disease with cardiovascular implications. It has been suggested that the pathogenesis involves nocturnal arousal, intermittent hypoxia after apnoeic episodes, and sympathetic activation and chronic inflammation (L. M. DelRosso et al., 2020). According to recent estimates, Moderate to severe dyspnoea caused by sleep is experienced by 3% to 23% of women and 9% to 49% of middle-aged men, respectively, and is characterised by an Apnoea-hypopnea index (AHI) of more than 15 episodes per hour of sleep recurrent obstruction of the upper airways as you sleep, which causes abrupt disturbances to blood oxygen levels, heart rate, blood pressure, intrathoracic pressure, and sleep quality, are the hallmarks of OSA. These short-term impacts have long-term consequences by lowering the quality of life, depressed mood, raise the risk of hypertension, cardiovascular disease, and early death, among other things (AlRumaih et al., 2018). According to reports, up to 90% of participants in these population-based research did not previously get a sleep Apnoea diagnosis from a doctor, despite the high incidence rates of OSA. Despite the widespread belief that public awareness of OSA has been rising consistently over the past three decades, this can be taken as hypothesis that general public awareness and knowledge of the condition are still lacking, which adds to the high number of undiagnosed OSA subjects in the community (Sia et al., 2017)
Recurrent episodes of apnoea during sleep, brought on by a brief loss of ventilatory effort, are the hallmark of Central Sleep apnoea. These apnoea are typically caused by the respiratory system's heavy reliance on the metabolic control system, specifically arterial PCO2 (White, 2005). Central apnoea occur when breathing stops without any obstruction to the airway. Central sleep apnoea (CSA) is commonly described as having a central Apnoea index (CAI) of at least one event per hour, with a CAI of at least five indicating severe disease (Judd et al., 2022). As a result, they can happen at any point during the wake-sleep transition: when waking PCO2 may be lower than sleeping levels and hence not stimulating to ventilatory effort; idiopathic Central Sleep apnoea, when high gain is coupled with prolonged circulation time (Cheyne-Stokes respiration); or hypercapnic respiratory failure, when PCO2 control mechanisms are malfunctioning. Whatever the underlying reason, central apnoea is frequently linked to arousal from sleep, which can result in insomnia during the day and difficulty falling asleep (White, 2005). About 25 to 40 percent of patients with chronic heart failure have Central Sleep apnoea, which is caused by cyclic hyperventilation and lowering in arterial carbon dioxide partial pressure that is below the apnoea threshold. The illness raises the risk of death on its own and has a detrimental effect on cardiovascular function through tissue hypoxia, arousals from sleep, and sympathetic nervous system activation (Ryan & Bradley, 2005).
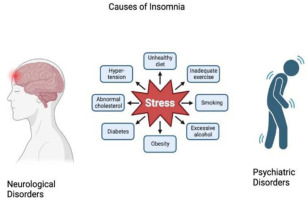
Having symptoms like trouble sleeping for two to three months straight, they are said to have Acute Insomnia. In fact, a few earlier research have shown that stress is linked to a variety of subjective and objective sleep disturbances (Elder et al., 2023) (Figure 4). Subsequently in a survey, a set of seventeen questions was administered to the participants to determine which ones had acute insomnia and whether they had any signs of co-occurring medical disorders or other sleep disorders. and participants were classified as having co-morbid acute insomnia if they provided an affirmative response to any of the questions (Ellis, Perlis, et al., 2012).
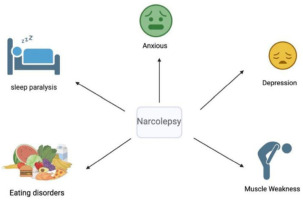
Narcolepsy can be defined as a chronic sleep disorder that includes excessive daytime sleepiness, cataplexy, frequent, uncontrollable sleep attacks, and abnormalities related to rapid eye movement sleep, hypnagogic or hypnopompic hallucinations and sleep paralysis (Witt et al., 2018). An additional feature of narcolepsy is abnormal regulation of Rapid-Eye Movement (REM) sleep (Mitler et al., 1987). It's important to take into account how REM sleep dysregulation, particularly cataplexy, affects social interaction and interpersonal relationships (Thorpy & Bogan, 2020). Studies using Continuous Electrographic Monitoring have demonstrated that narcolepsy is typified by a failure to maintain extended wakefulness or sleep that are normally proportioned. Therefore, a narcoleptic may spend 16 hours a day awake and 8 hours a day asleep, but during intended periods of wakefulness, they will frequently experience bouts of sleep and numerous arousals during intended periods of sleep (Mitler et al., 1987).
The physiology of the hypothalamic-pituitary-adrenal axis, glycolipid metabolism, and cardiovascular system are all negatively impacted by qualitative and/or quantitative sleep problems, which significantly raises the risk of cardiometabolic disease. In particular, there is unquestionably a strong correlation between sleep disturbances and arterial hypertension, cardiovascular illness, diabetes mellitus, and/or obesity, according to observational research and experimental data (the Italian Society of Hypertension (SIIA) et al., 2021) and sleep disorders do have a significant impact on hypertensive patients and also the main cardiovascular consequences linked to hypertension include myocardial infarction, heart failure, stroke, and death. Mechanical hemodynamic alterations, arterial stiffness, neurohormonal and vegetative abnormalities, dysregulation, and decreased renal function all worsen adverse outcomes (Isayeva et al., 2022). The systematic review aims to study 4 different types of sleep orders in detail (which includes their epidemiology, pathophysiology, diagnosis, symptoms and treatment) which are Sleep Apnoea, Insomnia, Narcolepsy and Restless Leg Syndrome. The DSM-IV and International Classification of Sleep Disorders covered these topics, which included narcolepsy, sleep-related breathing disorders, parasomnias, circadian rhythm disorders, restless legs syndrome, and 8-periodic limb movement disorder. Second Edition. Acute (transient), short-term (up to six months), and chronic (more than six months) sleep problems are all possible. Any person can get acute sleep disturbances as a result of stress, overexcitation, or time zone changes. People who are prone to sleeplessness develop chronic insomnia. (Tursunboyev, 2025)
2. METHODOLOGY
From January 2024 to November 2024, a systematic review was executed using Google Scholar database. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed. The Medical Subject Headings (MeSH) are as follows- “sleep disorders” and “hypertension” and “Cortisol Awakening Response”. A number of advanced search methods were used to carry out the review with filters focusing specifically on subject headings along with different types of sleep disorders which includes sleep apnoea, insomnia, narcolepsy and restless leg syndrome. Filters were applied according to years and exclusion and inclusion criteria was used with exclusion of case study articles and reviews. The articles and reviews were analysed individually and added to the review as shown in Figure 1.
2.1. Inclusion criteria
Studies related to different types of sleep apnoea and their pathophysiology and epidemiology.
Studies related to different types of Insomnia and its diagnosis and treatment.
Studies related to Narcolepsy, including its pathophysiology and treatment
Studies related to Epidemiology, Pathophysiology, Diagnosis, and treatment of Restless leg Syndrome.
Lifestyle modifications considered as part of the treatment for sleep disorders
Consideration of Covid-19 aspects in relation to obstructive sleep apnoea.
2.3. Explanation for inclusion and exclusion criteria
This review paper aims to understand the different types of sleep disorders and about their treatment, epidemiology, pathophysiology etc. As this paper doesn’t include the severity of each disease in detail or is not related to each disorder’s distribution, it was included in the exclusion criteria and this review paper cites and includes the pathophysiology, epidemiology, diagnosis, symptoms and treatment of 4 different types of sleep disorders i.e. Narcolepsy, Restless leg syndrome and different types of insomnia and sleep apnoea. This information has been reviewed from different types of articles taken within a range of 2002–2025 and is cited in this paper, hence this was all part of the inclusion criteria. This paper didn’t focus on the study designs used in different researches but rather on the lifestyle modification caused by the these diseases and their relation with Covid-19.
2.4. Data extraction
The epidemiology and pathophysiology of each disease was analysed separately from different papers which were carefully analysed using the advanced search using specific keywords on google scholar. Continuous positive airway pressure is dealt in more detail in sleep apnoea for example. In the rest the major studies include regarding how to treat parts of buccal cavity either surgically or naturally in order to reduce pressure and treat the disorders mentioned above gradually. The epidemiology considers different ranges of age and tells how the particular disorders increases or decreases as the age increases. The pathophysiology majorly considers which part of the buccal cavity is affected which causes the disorders and the mechanism in the part of the buccal cavity which ultimately leads to the disorder to be caused such as- Uvulopalatopharyngoplasty (UPPP) for treatment of Obstructive sleep Apnoea.
3. RESULTS AND DISCUSSION
The search approach used in this systematic review is shown in the PRISMA flow diagram. The Google Scholar databases yielded 92 publications in total. From those, 40 articles were evaluated for eligibility after duplicates were eliminated. Additionally, out of 40 publications, 20 were accessible in full-text, and 12 were ultimately included in the systematic review after taking the inclusion and exclusion criteria into account.
Table 1 talks about the complications caused by Obstructive Sleep Apnoea which includes cardiovascular risks, surgical wound implications, vitamin d deficiency and in chronic cases kidney transplantation (Protasiewicz Timofticiuc et al., 2022); (Ozdilekcan et al., 2021); (Loh et al., 2023); (Kanbay et al., 2023), Table 2 talks about studies of the 4 different sleep disorders (which this systematic review talks about) in general where a single paper or review targeting that particular disorder is taken and the findings and purpose of the paper is talked about in a very brief manner (Marquina et al., 2023); (Suraev et al., 2020); (Streatfeild et al., 2021). Tables 3 and 4 talk about interventions and specific techniques to treat the 4 different sleep disorders which includes therapies, drugs and relaxation techniques used to treat these disorders in a little more detail (Aardoom et al., 2020); (De Crescenzo et al., 2022); (Franceschini et al., 2020); (Ratnani & Harjpal, 2023); (Golovatyuk & Poluektov, 2023). Table 5 talks about symptoms caused by these sleep disorders in general along with their description (Chidambaram et al., 2022); (Bartolucci et al., 2023); (Protasiewicz Timofticiuc et al., 2022)
Table 1
Complications due to Obstructive sleep Apnoea.
| S. No. | Complications | Study result | References |
|---|---|---|---|
| 1 | Cardiovascular risks: OSA is linked to an increased risk of coronary heart disease (CHD) and stroke, as shown in a study including type 2 diabetic patients (T2DM) | A STOP-Bang score of ≥5 was found to be associated with a 10-year risk of both fatal and nonfatal coronary heart disease. | (Protasiewicz Timofticiuc et al., 2022) |
| 2 | Surgical wound complications: Individuals who are at a high risk of developing OSA syndrome may face respiratory difficulties following surgery. | None | (Ozdilekcan et al., 2021) |
| 3 | Vitamin D deficiency: Individuals who are at a high risk of developing OSA syndrome may face respiratory difficulties following surgery. | None | (Loh et al., 2023) |
| 4 | Kidney transplantation: Patients with chronic renal disease often report having OSA, and a kidney transplant does not statistically significantly alter the Apnoea-hypopnea index or the amount of time these patients spend sleeping. | In order to improve primary and secondary prevention of cardiovascular events, it is | (Kanbay et al., 2023) |
Table 2
Study of Sleep disorders.
| Topic | Title | Purpose | Findings | References |
|---|---|---|---|---|
| Sleep Apnoea | The preventable productivity burden of sleep Apnoea in Australia: a lifetime modelling study | Determine the productivity burden of OSA in Australia using productivity-adjusted life-years (PALYs) | The Australian population with OSA accrued 193,713,441 years of life lived and 182,737,644 PALYs | (Marquina et al., 2023) |
| Insomnia | Cannabinoid therapies in the management of sleep disorders: A systematic review of preclinical and clinical studies | Provide a systematic review of preclinical and clinical studies on cannabinoid therapies in the management of sleep disorders | Promising preliminary evidence provides the rationale for future randomized controlled trials of cannabinoid therapies in individuals with insomnia | (Suraev et al., 2020) |
| Narcolepsy | Cannabinoid therapies in the management of sleep disorders: A systematic review of preclinical and clinical studies | Provide a systematic review of preclinical and clinical studies on cannabinoid therapies in the management of sleep disorders | There is a clear need for further investigations on the safety and efficacy of cannabinoid therapies for treating narcolepsy using larger, rigorously controlled, longer-term trials | (Suraev et al., 2020) |
| Restless Leg Syndrome | The Social and Economic Cost Of Sleep Disorders | Estimate the economic cost of common sleep disorders in Australia for 2019-2020 | The estimated overall cost of RLS in Australia in 2019-2020 was $9.0 billion | (Streatfeild et al., 2021) |
Table 3
Interventions and their effectiveness.
| Intervention | Type of disorder | Effectiveness | Reference |
|---|---|---|---|
| ContinuousPositive airway pressure | SleepApnea | Highly effective for normalizing breathing and sleep; it reduces the frequency of respiratory events during sleep | (Aardoom et al., 2020) |
| Pharmacological treatments | Insomnia | ImproveInsomnia andSleep quality | (De Crescenzo et al., 2022) |
| Pitolisant is a new wake-promoting agent that can be used as an intervention | Narcolepsy | Wake-promoting agent | (Franceschini et al., 2020) |
| Medications like gabapentin and pregabalin | Restless legSyndrome | Treats the symptoms of RLS and enhances sleep | (Ratnani & Harjpal, 2023) |
Table 4
Techniques to treat Sleep disorders.
| Treatment | Description | References |
|---|---|---|
| Cognitive Behavioural Therapy for Insomnia (CBT-I) | A prominent nonpharmacologic treatment for insomnia, effective for both primary and comorbid insomnia. It is the most effective method for treating chronic insomnia with a sustained effect. Remote methods of CBT-I are becoming increasingly relevant, offering the possibility of use by a wide group of people and showing comparable effectiveness to full-time CBT-I | (Golovatyuk & Poluektov, 2023) |
| Sleep hygiene | A set of habits and practices that promote healthy sleep, such as maintaining a regular sleep schedule, avoiding caffeine and alcohol before bedtime, and creating a comfortable sleep environment | (Golovatyuk & Poluektov, 2023) |
| Relaxation techniques | Activities that promote relaxation and reduce stress, such as deep breathing, progressive muscle relaxation, and guided imagery | (Golovatyuk & Poluektov, 2023) |
| Light therapy | Exposure to bright light in the morning or evening to help regulate the body's circadian rhythms | (Golovatyuk & Poluektov, 2023) |
Table 5
Symptoms of Sleep disorders.
| Symptom | Description | References |
|---|---|---|
| Excessive daytime sleepiness | Feeling very sleepy during the day, even if you have had enough sleep at night | (Chidambaram et al., 2022) |
| Loud snoring | Making loud or disruptive snoring sounds while sleeping | (Chidambaram et al., 2022) |
| Episodes of breathing cessation during sleep | Pauses in breathing or instances of shallow or infrequent breathing during sleep | (Bartolucci et al., 2023) |
| Waking up with a dry mouth | Waking up with an unusually dry mouth or sore throat | (Bartolucci et al., 2023) |
| Morning headache | Waking up with a headache | (Bartolucci et al., 2023) |
| Difficulty staying asleep (insomnia) | Having trouble staying asleep | (Bartolucci et al., 2023) |
| Attention problems | Having difficulty paying attention while awake | (Protasiewicz Timofticiuc et al., 2022) |
3.1. Obstructive sleep apnoea
3.1.1. Introduction
A total of thirty-seven themes were prioritized and debated. The cost-effectiveness of management strategies, defining age- and sex-specific criteria for OSA, evaluating routine preoperative screening for OSA, evaluating the involvement of a sleep medicine specialist in OSA diagnosis, evaluating clinical prediction rules, comparing treatments for patients who cannot tolerate positive airway pressure, evaluating strategies to improve treatment compliance, and assessing the relationship between the severity of sleep Apnoea and long-term clinical outcomes were the nine highest priority FRN topics (Patel et al., 2013). The Apnoea-hypopnea index (AHI) can be used to classify the severity of OSA as mild, moderate, or severe. The number of episodes of apnoea and hypopnea that happen during sleep determines your AHI. The total pause in breathing for longer than 10 seconds is known as Apnoea, while the partial cessation of breathing is known as hypopnea. Mild OSA lasts for five to fifteen seconds whereas, moderate OSA lasts for fifteen to thirty seconds, and severe OSA lasts for more than thirty seconds (AlRumaih et al., 2018). Obese people, the elderly, and men are more likely to experience sleep obstructions, APN. The most significant of these factors is obesity, which affects around 70% of people with this condition is on the rise, particularly in industrialised nations and is the only significant modifiable risk factor (Ho & Brass, 2011). Table 1.
3.1.2. Comparison between Osa and Covid-19
Given that individuals who have recovered from COVID-19 have significant changes in their pulmonary performance, it is reasonable to believe that these pulmonary aftereffects could exacerbate OSA. Although the precise method by which respiratory system disruptions result in sleep disorders is yet unknown, the following suggestion can be made: Breathlessness has been associated with changes in lung function and alveolar epithelial cells in subjects recovered from SARS-CoV-2 infection (Ozdilekcan et al., 2021).
3.1.3. OSA and Vitamin-D
There may be a distinct association between vitamin D and OSA since patients with OSA, regardless of age or BMI, have lower serum 25-OHD levels and a higher frequency of vitamin D deficiency. Additionally, OSA can negatively impact various aspects of health, including surgical outcomes and vitamin D levels, highlighting the importance of addressing this condition in clinical practice (Kanbay et al., 2023; Loh et al., 2023).
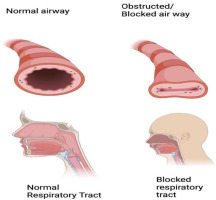
3.1.4. Pathophysiology
The pharyngeal airway in majority of mammals is supported by a solid skeleton, the human upper airway's patency is mostly preserved by soft tissue structures and muscle action. Pharyngeal imaging (CT and MRI) performed during waking provides the basis for most theories of the pathophysiology of obstructive sleep apnoea. These images show that individuals with this disorder have smaller upper airways than normal age- and weight-subjects (Malhotra & White, 2002). Progressive expiratory narrowing in the retro palatal area is a significant factor in upper airway obstruction during sleep, even though negative collapsing pressure during inspiration is frequently the cause. In contrast to individuals without apnoea, patients with Apnoea mainly have smaller or less functional pharyngeal systems (Malhotra & White, 2002).
Pharyngeal patency is facilitated by increased transmural pressure, whereas pharyngeal collapse is facilitated by decreased pressure. The closing pressure is the transmural pressure at which there is no more pharyngeal area. As the pharynx's luminal area shrinks, it becomes more vulnerable to collapse (Qureshi, 2003).Periodic or non-periodic pharyngeal narrowing are both possible. A persistent rise in airflow resistance occurs with nonperiodic blockage, either with or without concomitant desaturation. This persistent rise resistance had been called upper airway resistance syndrome because it might cause sleep disturbance and somnolence during the day (Qureshi, 2003). The pharynx may be more susceptible to collapse due to factors such as the existence of soft tissues and bony structures, which increase extraluminal tissue pressures, and negative pressure within the airway; however, the pharynx's dilator muscles' tonic and phasic contractile activity helps to maintain pharyngeal patency. Patients with sleep disordered breathing experience recurrent upper airway obstructions due to an imbalance between these opposing forces (Mannarino et al., 2012).
The dilator muscles of the upper airways of an apnoea patient need to be significantly in greater activity during waking in comparison to those of healthy controls in order to overcome altered pharyngeal architecture. Compared to healthy controls, patients with obstructive sleep Apnoea showed significantly higher genioglossal activation during waking, according to recent research using quantitative electromyographic comparisons between individuals (Malhotra & White, 2002).There are several other anatomical factors which assist OSA. These consist of the patient's sleeping posture, airway responsiveness, and secretions. Position can significantly affect the patency of the airways (Ho & Brass, 2011). This higher negative pressure causes more muscle activation since the incline of the relationship between activation and negative pressure is comparable in patients with obstructive sleep apnoea and in healthy individuals. Apnoea patients exhibit higher levels of tonic (basal, non-inspiratory) muscle activity in these regions compared to individuals in good health (Ho & Brass, 2011).
3.1.5. Epidemiology
The OSA prevalence is still very high in the elderly, and after menopause, the gender differences become much less pronounced. The prevalence of at least moderate OSA (AHI ≥ 15) varies greatly among the elderly, with studies using different methodologies reporting prevalence as low as 7% to as high as 44%. But why the middle-aged population's consistent rise in OSA prevalence plateaus at age 65 is still a mystery (Lee et al., 2008).The Sleep Heart Health Study showed that the prevalence of OSA peaked at age 60 and that middle-aged adults, particularly men, are primarily at risk for all-cause and cardiovascular mortality when they have OSA. Research indicates that the AHI is less affected by BMI in older adults than in middle-aged adults. Additionally, changes in BMI, especially those associated with weight gain, are less notable in this age group (Lee et al., 2008).
OSA is defined as five or more incidents per hour. 425 million adults between the ages of 30 and 69 have moderate to severe OSA (15 or more events per hour), which is a condition that affects 1 billion people globally. According to reports, 9–17% of women and 25–30% of men in the US fit the criteria for obstructive sleep apnoea
3.1.6. Symptoms
Common night-time symptoms include gasping, snoring, witnessed apnoea, choking, and snorting. Dyspnoea, diaphoresis, restlessness, and dry mouth drooling.
Common daytime symptoms: Daytime sleepiness and fatigue, Impaired memory and concentration and Personality changes (Irritability, Aggressiveness, Depression, Anxiety) (Qureshi, 2003)
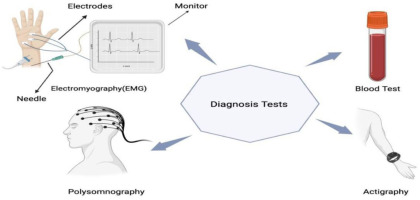
3.1.7. Diagnosis
The nightly Polysomnogram is considered the gold standard for diagnosing OSA. Recordings of respiratory effort, Oral and Nasal Airflow, Oxygen Saturation, Electroencephalogram, Electro-oculogram, Electromyogram, and leg movements are all included. A complete Polysomnogram may help to find the type of sleep that is occurring as well as the degree of OSA (Qureshi, 2003).Nasal pressure measurements can also be useful in detecting more subtle respiratory events and high inspiratory resistance. The findings of numerous studies indicate that when it comes to detecting respiratory events while you sleep, nasal pressure has a higher sensitivity than a Thermistor. Nevertheless, it's still unclear if this device's specificity is superior. Some have questioned the clinical significance of these minute events that are only picked up by measuring nasal pressure (Malhotra & White, 2002).
Split-night polysomnograms usually enable more rapid diagnosis and less expensive OSA treatment (Qureshi, 2003) there would be less benefit from split-night studies if auto titrating positive pressure devices were widely used at home, which would increase the amount of home-based diagnosis and treatment. Split night studies, however, are a useful strategy recent past (Malhotra & White, 2002).Numerous home diagnostic techniques have been studied or are currently being researched; the majority only measure respiratory signals. The existing systems vary greatly, ranging from two-channel (snoring and oximetry) to four-channel (oximetry, airflow, effort, and position), to full polysomnogram. These tests typically have an 80% diagnostic accuracy rate; as the number of channels increases, the accuracy increases along with the complexity (Malhotra & White, 2002)
Assessment of suspected OSA may also involve home cardiorespiratory studies. Heart rate, breathing effort, airflow, and oxygen saturation are typically tracked in these investigations. These tests are helpful for screening, but they typically don't reveal anything about the architecture of sleep and may not be able to distinguish between being awake and asleep. Thus, it may be challenging to diagnose upper airway resistance syndrome and even mild sleep Apnoea. Only nocturnal desaturation is revealed by overnight Oximetry, which does not serve as a replacement for a Polysomnogram (Qureshi, 2003).
3.1.8. Treatment
Treatment includes Positional therapy, weight loss, oral appliances, continuous positive airway pressure (CPAP), treatment of nasal allergies, exercise and surgery (Sia et al., 2017).
Lifestyle modification: The need of weight loss should be emphasized for people with OSA who are overweight or obese. Losing weight is usually not curative, but it is advised and can frequently lessen the degree of obstructive sleep apnoea. Patients should prioritise getting at least 7 to 8 hours of sleep every night and be informed about the relationship between sleep duration and health. This entails advising patients to stop using sedatives, alcohol, and tobacco, lose weight, and avoid sleep deprivation (Qureshi, 2003). Positional therapy may be administered alone or in conjunction with CPAP to a specific subset of patients. Patients receiving this type of therapy typically sleep with their heads propped up at an angle of 30° to 60° or in the lateral position. Positional therapy usually minimizes total frequency of apnoea by stabilising the pharynx. Patients with milder OSA and mild to non-existent obesity are more likely to benefit from positional therapy. Nasal dilators, electrical stimulation of the upper airway, and medications like Protriptyline and Mirtazapine have all been tried to treat OSA, but none of them have been able to sufficiently lower apnoea. Therefore, it is not currently advised to use these therapies widely (Qureshi, 2003).
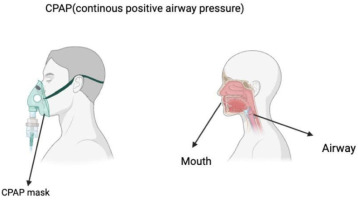
CPAP: The gold standard of treatment is CPAP. In 1980, Dr. Sullivan created the first CPAP gadget. By raising the airway pressure above the point at which the upper airway collapses, the pneumatic support used by CPAP machines preserves upper airway patency (AlRumaih et al., 2018). Reductions in daytime sleepiness, mood disturbances, and cognitive impairment are among the symptoms of OSA that are strongly correlated with lowering the apnoea hypopnea index. By applying air under positive pressure through a nasal or facial mask, it treats apnoea-hypopnea by forming a pneumatic splint in the pharynx that keeps the pharyngeal airway from collapsing (Qureshi, 2003). Reductions in daytime sleepiness, mood disturbances, and cognitive impairment are among the symptoms of OSA that are strongly correlated with lowering the apnoea hypopnea index (Salman et al., 2020) (Figure 2)
Oral appliances: OAs provide reversible, easy, and affordable treatment for OSA, snoring, or both. Three primary categories can be used to categorise OA therapy: soft palate lifters, tongue retaining devices (TRDs) that realign the tongue forward, and mandibular advancement appliances (MRAs) that move the mandible forward during sleep (AlRumaih et al., 2018). Most mouthpieces on the market are only authorised to treat snoring. The US Food and Drug Administration has only permitted fourteen devices for the treatment of OSA. Out of these, only three had undergone regulated or randomised Clinical checks, and only seven are adjustable, allowing for mandibular titration. The idea behind these devices is to increase space in the posterior pharyngeal area by mechanically moving the tongue or the jaw and tongue forward (Qureshi, 2003). Patients generally favour them over continuous positive airway pressure (CPAP). Therefore, patients who have not responded to surgery or who have refused CPAP therapy should also be evaluated for oral appliances (Malhotra & White, 2002)
Surgery: Patients with OSA who have distinct craniofacial abnormalities are probably better candidates for surgical intervention than patients who are just obese. There are numerous options for procedures, many of which target the obstruction's location (Qureshi, 2003). In many parts of North America, when it comes to surgical options, UPPP is regarded as the primary or first-stage surgical treatment for OSAS. In 1981, Fujita et al. published the first description of Uvulopalatopharyngoplasty (UPPP) (Goodday, 2009) which involves the resection of the soft palate's redundant soft tissue and uvula. Merely 41% of patients undergoing the procedure experience less than 20 occurrences per hour as the AHI. Furthermore, given the hazy relationship between AHI and apnoea complications, 20 events per hour is not always regarded as a satisfactory surgical result. Furthermore, there is no proof that physical examination or imaging procedures help patients make better surgical decisions (Malhotra & White, 2002).
There can be at least two distinct stages to a surgical procedure. All the listed procedures, except for maxillomandibular advancement, can be combined during phase I surgery. When these procedures are combined, the reported short-term response rate is roughly 60%. Maxillomandibular advancement surgery is part of Phase II surgery that may be considered if the patient does not respond (Qureshi, 2003). The combined Phase I and II surgical success rate can reach 90% in certain patients. If the patient is overweight, has severe OSA, and oxygen desaturation is less than 70%, the success rate is probably lower. Following maxillomandibular advancement, complications may include bleeding, hematomas, upper airway obstruction from surgical oedema, and facial anaesthesia (Qureshi, 2003). A tracheostomy may be the last resort if all other treatment options are ineffective, particularly in morbidly obese patients who have severe OSA, severe oxygen desaturation, and/or concomitant cardiac disease (Qureshi, 2003).
3.2. Central sleep apnoea
3.2.1. Introduction
Overall, CSA is far less common than obstructive sleep apnoea (OSA); In a recent study conducted in the community, where sleep disordered breathing was highly prevalent, central disordered breathing events accounted for a very small portion of all sleep disordered breathing events. However, certain subpopulations, like those with heart failure, those receiving long-term opioid therapy, and those ascending to high altitudes—have higher prevalence rates of particular CSA disorders. Furthermore, there is a growing awareness and examination of TE-CSA (Treatment emergence CSA) due to the high incidence of OSA and the steadily rising count of patients undergoing continuous positive airway pressure (CPAP) therapy. Sleep fragmentation, frequent awakenings, oxyhaemoglobin desaturations, and daytime sleepiness are all potential effects of CSA (Hernandez & Patil, 2016). At high altitudes, Central Sleep apnoea (CSA) usually consists of 2-3 breaths interspersed with an apnoea between each burst, which visually mimics the periodic breathing of a premature infant (Burgess & Ainslie, 2016). It happens at elevations over 2000 m with variable severity based on individual characteristics, but it happens to most people above 5000 m (Roach, Hackett, & Wagner, 2016). Table 2 represents the various sleep disorders.
3.2.2. Pathophysiology
The pathophysiology of which, arising from pharyngeal occlusion, differs from that of Central Sleep apnoea (Ryan & Bradley, 2005). During such an apnoea, a total cessation of electromyographic activity of the breathing muscles would be predicted, and this has been shown, since central apnoea are defined as breathing pauses without ventilatory effort. The normal muscular activity of the ventilatory system resumes after the apnoea. This result suggests that during central apnoea, the neuronal output to the respiratory muscles stops and then resumes at the conclusion of the ventilatory pause (White, 2005). It has previously been suggested that there is a physiological pathway linking high altitude sleep and CHF that results in breathing instability when you sleep. Other potential causes of central apnoea include technical issues with excessive PAP titration, mask leaks, and a decrease in sleep quality as a result of PAP initiation increasing state stability and causing central apnoea to occur during the sleep-wake transition (Pagel et al., 2011).
3.2.3. Epidemiology
Bixler et al. showed that older adults had a higher central apnoea index (12.1% vs. 1.8%) than middle-aged adults (Qureshi, 2003). When people age, the prevalence of CSA tends to rise, and it is more common in older adults over 65. A cross-sectional study that used an adapted version of the ICSD-3 classification found that 2.7% of men 65 years of age and older had CSA. AHI ≥ 10 represented 38 and 33 patients with OSA and CSA-CSR (Cheyne Stokes respiration), AHI ≥ 15 represented 32 and 29%, and AHI ≥ 20 events/h represented 27 and 25% of patients, respectively. Risk variables for CSA-CSR included male gender, age N60, atrial fibrillation, and awake PaCO2 ≤38 mm Hg. Men with a BMI of at least 35 kg/m2 and women over 60 years of age were at risk for OSA (Naughton, 2016). When people age, the prevalence of CSA tends to rise, and it is more common in older adults over 65. A cross-sectional study that used an adapted version of the ICSD-3 classification found that 2.7% of men 65 years of age and older had CSA (Rana, 2023). In a recent large sample study using real-life population-based data, Liu et al. looked at telemonitoring device data for the presence or absence of emergent CSA at baseline (week 1) and week 13. Patients (133,006) had at least one day of at least one hour use of CPAP during weeks one and thirteen. 3.5% of patients had CSA in either week 1 or week 13; of these, 55.1%, 25.2%, and 19.7%, respectively, had transient, persistent, or emergent CSA (J. Zhang et al., 2020).
3.2.4. Common mechanisms of central sleep apnoea syndromes
Ventilatory control instability: The main pathophysiological mechanism of the subset of central apnoea syndromes marked by eucapnia or hypocapnia during wakefulness is ventilatory control instability (Hernandez & Patil, 2016). Introducing the idea of “loop gain” will help you better understand this (White, 2005). Ventilatory control is dependent on two general conditions: a narrow CO2 reserve and a high loop gain system. The respiratory system is more vulnerable to instability and potential oscillation between central apnoea and hyperventilation when these factors are combined. In contrast, a low loop gain system will react more slowly and with a smaller magnitude to a given disturbance, a high loop gain system will respond quickly and strongly (Hernandez & Patil, 2016).
Loop gain: Loop gain can be divided into controller gain and plant gain:
A. Controller gain: Chemosensitivity, or the ventilatory response to a hypoxic or hypercapnic disturbance, is referred to as controller gain. More specifically, it refers to the extent of minute ventilation rise for a specific disturbance (PaCO2 or PaO2). A person with a high controller gain will exhibit a higher ventilatory response, which will increase the risk of hypocapnia. A person with normal controller gain will likely experience mild hypocapnia or eucapnia due to a more attenuated ventilatory response (Hernandez & Patil, 2016). The ventilatory control system's responsiveness, mostly to variations in PCO2 but also, to a lesser degree in Po2 (White, 2005).
B. Plant gain: The term “plant gain” describes how much the PaCO2 changes in reaction to a modification of minute ventilation. A high plant gain individual will show a comparatively big change in PaCO2 for a given change in minute ventilation, conversely, a poor plant gain individual will see a lesser change in PaCO2. A number of variables, such as lung volume and baseline CO2 level, influence plant gain (Hernandez & Patil, 2016). The effectiveness of the lung apparatus's (parenchyma and respiratory muscles) removal of CO2 from the body (White, 2005).
Upper airway obstruction: The upper airway frequently occludes entirely or partially during a central apnoea, most likely as a result of a decline in the central drive to the muscles that dilate the upper airway. Furthermore, during inspiration, a ventilatory overshoot may occur as the increased upper airway resistance resolves, which can lead to hypocapnia and central apnoea. Although direct human observations of this have not been made, indirect evidence points to this mechanism as a potential contributing factor. Compared to snorers without CSA, snorers with CSA were found to have higher pharyngeal compliance (Hernandez & Patil, 2016) (Figure 3)
3.2.5. Types of CSA
3.2.5.1. Non hypercapnic CSA
A. Normal central apnoeic events
When the wakefulness drive to breathe is gone, the PaCO2 is frequently at or less than the apnoeic threshold during the shift from wakefulness to sleep onset, which causes a central apnoea. Furthermore, spontaneous arousals and sigh breaths during normal sleep cause ventilation to increase and frequently lower eucapnic PaCO2 levels below the apnoeic threshold (Hernandez & Patil, 2016).
B. High altitude CSA
Periodic breathing, or high-altitude CSA, is the term used to describe the onset of central apnoea during sleep at an altitude (Hernandez & Patil, 2016). When the altitude is high enough, this phenomenon happens to everyone, but it usually happens at elevations higher than 15,000 feet (4572 metres) (Hernandez & Patil, 2016). The reduced partial pressure of atmospheric oxygen, which causes hypoxia and raises minute ventilation, is the primary cause of high-altitude cerebral suffocation. As a result, there is a decrease in PaCO2 and hyperventilation, which brings the wakefulness eucapnic PCO2 nearer the threshold of apnoea and lowers the CO2 reserve. This, along with a potential increase in apnoeic threshold brought on by hypoxia (which lowers the CO2 reserve even more), predisposes to central apnoea at the onset of sleep and subsequent ventilatory instability, which manifests as a hyperventilation and apnoea cycle (Hernandez & Patil, 2016).
Idiopathic CSA: Idiopathic CSA is a rare condition that, by definition, only occurs at sea level in people who do not have any significant neurological, cardiac, or renal disease, and it has nothing to do with treatment using positive pressure. In idiopathic CSA, the cycling period lasts between 30 and 40 seconds, and it seems to be mostly caused by increased PCO2 chemosensitivity (Orr, 2016). Arousals usually take place at the height of hyperventilation and are thought to be involved in ventilatory overshoot, which improves chemo-responsiveness. A narrow CO2 reserve combined with a high loop gain state is thought to be the main mechanism (Hernandez & Patil, 2016).
3.2.6. Cheyne-Stokes breathing- symptoms
Cheyne-Stokes breathing (CSB) is a specific symptom of Central Sleep apnoea, though it can also occur without meeting the diagnostic requirements. An increasing-decreasing respiratory trend of waxing and waning hyperpnea's divided by central hypopneas or apnoea is specifically referred to as CSB. Sleep-wake instability, narrow low CO2 reserve, and high controller gain are the main causes of the ventilatory instability of CSB (Hernandez & Patil, 2016). The hallmarks of Cheyne-Stokes respiration (CSR) include a crescendo-decrescendo pattern of hyperventilation interspersed with apnoea or hypopnea, which happens at the nadir of the pattern during sleep (particularly shallow sleep, like sleep stages 1 or 2) and occasionally during waking hours (Maestri et al., 2019). The difference in time domain technique was used to measure the lung-to-ear delay and the lung-to-finger delay (i.e., the delay between tidal volume and SpO2_Ear and SpO2_Finger, respectively). This method makes it possible to assess the time lag brought on by distortion effects in addition to the pure transport delay. This correlation validates the findings of previous research in heart failure patients with Central Sleep apnoea (L. DelRosso & Bruni, 2019).Congestive heart failure has long been linked to Cheyne-Stokes breathing both while awake and when asleep. A ventilatory rhythm that rises and falls, with a central apnoea or hypopnea at the lowest point characterises this breathing pattern. This is not the same as the more sudden onset and resolution of idiopathic central Apnoea, as previously mentioned. A prolonged circulation time and increased ventilatory responsiveness to rising PCo2 combine to produce ventilatory control system instability (high loop gain), which is nearly solely responsible for this breathing pattern (White, 2005).
In rhythm production, where opioid receptors are highly expressed, Kolliker-Fuse neurons are also involved. Breathing rate suppression is another effect of directly administering opioid agonists to the KF/PB neurons. Pre-Böt Com receives descending inputs from a variety of sources, including pontine KF/PB nuclei, as should be emphasized. The suppression of breathing and the activation of ataxic breathing and CSA seem to be coordinated by neurons in both nuclei. (Javaheri et al., 2024)
3.2.7. Treatment
CPAP expands lung volume, which enhances CO2 damping and lowers plant gain (Orr et al., 2017).
Additional oxygen improves CSA in certain heart failure patients and has a significant effect on CSA in new-borns and at altitude. It is well known that elevated arterial PO2 reduces carotid body chemo-sensitivity (Orr et al., 2017).
Inhaled carbon dioxide, breathing again, Acetazolamide, and Theophylline are examples of respiratory stimulants that act to increase CO2 damping (reduce “plant gain”) by lessening the sensitivity of alveolar PCO2 to changes brought on by variations in ventilation (Orr et al., 2017).
Sleeping position - elevating the bed or sleeping on one side can enhance CSA, possibly due to increased lung volume (Orr et al., 2017).
To address CSA, dynamic interventions aim to clamp ventilation or PCO2 levels. Examples of these include dynamic inspired CO2 delivery and adaptive servo-controlled ventilation (Orr et al., 2017).
3.2.8. Diagnosis
Patients on opioids may experience CSA, which can manifest as either a periodic or more ataxic pattern (CSA brought on by a drug or substance). In addition, patients with myopathies and those with other respiratory or sleep-related breathing disorders, such as congenital central hypoventilation syndrome, may also experience CSA (Morgenthaler et al., 2021). The two main factors influencing the clinical characteristics of hypercapnic central apnoea are the underlying disease process and the frequency of sleep-related apnoea. These include symptoms of sleep apnoea syndrome, such as daytime sleepiness, snoring, poor nocturnal sleep, and morning headaches, as well as symptoms of the underlying condition, such as weakness and dyspnoea (Badr & Javaheri, 2019).
The typical symptoms of sleep apnoea syndrome can be seen in patients with non-hypercapnic central apnoea, although they typically do not support subjective daytime sleepiness. For central apnoea, a full-night in-laboratory Polysomnography is the gold standard diagnostic procedure. It is considered clinically noteworthy when at least five central events are found in an hour. The minimal number of events necessary to trigger a particular illness or condition is yet unknown and may vary depending on the patient population. Therefore, there is no cut-off point for the quantity of central apnoea linked to illness (McLaren et al., 2019). Using Polysomnogram these parameters are measured: Heart rate, airflow monitored by Side stream End-Tidal Capnography, which also provided breath-by-breath assessments of end-tidal carbon dioxide levels, nasal pressure, and an oronasal thermistor, were measured along with the chest and abdominal wall movements. >90% reduction in airflow without thoracic or abdominal movement and at least one of the following characteristics was considered a central apnoea: Either the event lasts for twenty seconds or more, is connected to an awakening, an arousal, or an oxygen desaturation of less than three percent (Judd et al., 2022).
4. CHRONIC INSOMNIA
4.1. Introduction
The International Classification of Sleep Disorders, whose diagnostic standards are comparable. According to these requirements, symptoms must result in functional distress or impairment that is clinically significant; must exist for a minimum of three nights a week for a minimum of three months, and it must not be connected to any other sleep, health, or mental disorders (Qaseem et al., 2016). Chronic insomnia disorder affects 6% to 10% of people (Mysliwiec et al., 2020) (Figure 4). When there is enough opportunity and conducive conditions for sleep, but difficulties with the onset, maintenance, the beginning, or quality of sleep impairs daytime functioning, it is referred to as insomnia. The majority of research studies use arbitrary definitions, such as a sleep efficiency of less than 85% or a sleep onset delay of more than thirty minutes (Silber, 2005). It is characterised as discontent with the amount or quality of sleep and is linked to problems falling asleep, staying asleep, and waking up early in the morning and not being able to go back to sleep (Qaseem et al., 2016). Its effects on quality of life as well as the psychological, occupational, and economic domains demonstrate how burdensome it is for patients and the healthcare system. Due to obstacles to diagnosis and treatment, insomnia is frequently undiagnosed and untreated (Morin & Benca, 2012).Comorbid insomnia may go untreated even after it is identified because other medical or psychological issues frequently take precedence. Many approaches to treating insomnia have been developed, such as medication, sleep environment modifications, and cognitive behavioural therapy (Bragg et al., 2019).
4.2. Diagnosis
A number of criteria are proposed to diagnose insomnia, despite the lack of defined quantitative definitions. The average reported sleep latency of over thirty minutes, the amount of time spent alert after falling asleep that exceeds thirty minutes, sleep efficiency below 85%, and total sleep time of less than 6.5 hours are some examples of these. The existence of distress, daytime repercussions, or both is essential for the diagnosis of insomnia. People who complain about having trouble falling asleep at night but are not impaired during the day may just be short sleepers (Saddichha, 2010). Based on the traditional signs of insomnia linked to daytime impairment, an official diagnosis of sleeplessness was established. Additionally, a patient received the Patient Health Questionnaire-9 (PHQ-9). Her score of 14 out of 27 on the PHQ-09 indicated that she also had moderate depression (Bragg et al., 2019).
After ruling out a number of other conditions as the primary cause of sleep disturbances, including psychiatric (depression and anxiety), medical (pain), circadian (phase-delay syndrome), or other sleep disorders (restless legs syndrome/periodic limb movements, sleep-breathing disorders), the diagnosis of primary insomnia is essentially made by exclusion. When a sleep disturbance is determined to be directly and temporally linked to another mental, physical, or sleep problem, comorbid insomnia is diagnosed (Morin & Benca, 2011).The DSM-5 and ICSD-3 criteria require a subjective report of a sleep complaint (difficulty falling asleep, staying asleep, or waking up early) occurring at least three times a week for three months, along with at least one related daytime impairment (fatigue, attention impairment, mood disturbance, or impaired performance), in order to diagnose chronic insomnia (Saddichha, 2010).
4.3. Treatment
General patients
Evidence of a moderate calibre demonstrated that CBT-I enhanced treatment response, remission, wakefulness following the general population's sleep onset, efficiency, and quality. In the general population, stimulus control improved sleep onset latency and total sleep time, according to low-quality evidence (Qaseem et al., 2016).
Older patients
Evidence of low-to-moderate quality showed that CBT-I enhanced older people' sleep efficiency, wakefulness following sleep onset, and sleep onset latency. Moderate-quality evidence also demonstrated that CBT-I improved Insomnia Severity Index (ISI) and Pittsburgh Sleep Quality Index (PSQI) scores when compared with controls (Mysliwiec, 2020).
Pharmacologic treatment
Evidence was insufficient to determine the benefits of pharmacologic therapy with Benzodiazepines in the general population or in older adults (Mysliwiec et al., 2020). The behavioural elements of teaching stimuli control and good sleep hygiene (creating a consistent sleep environment and strengthening the link between it and sleep), Relaxation Therapy, Counter arousal techniques, and Sleep Restriction Therapy (restricting the amount of time spent in bed to sleep, then gradually raising the time of bed as sleep efficiency increases) are some examples of behavioural components. Components of cognitive therapy focus on unhelpful ideas and attitudes regarding slumber (Mysliwiec et al., 2020). Benzodiazepines, Benzodiazepine-Receptor agonists, and sedating antidepressants are among the prescription drug classes used to treat insomnia. The FDA has approved the use of long, intermediate, and short half-lived benzodiazepines for treating insomnia, while it has approved the use of intermediate, short, and ultrashort half-lived benzodiazepine-receptor agonists (Silber, 2005).
In patients with primary insomnia, a 14-day trial comparing trazodone, zolpidem, and placebo revealed that trazodone improved sleep latency and duration (measured by a questionnaire) compared to placebo, but zolpidem had a greater effect (Silber, 2005). For patients who are having trouble falling asleep or who wake up during the night and need to take a medication, Zaleplon is an alternative to zolpidem (Bragg et al., 2019).
Doxepin, a tricyclic antidepressant, was used to treat primary insomnia in a four-week study. The results showed significant improvements in sleep efficiency (13 percent increase from baseline), total sleep time (13 percent increase from baseline), and sleep latency (21 percent reduction from baseline) (Silber, 2005). the FDA advises women and elderly or disabled adults to take benzodiazepine and nonbenzodiazepine hypnotics at lower dosages (Qaseem et al., 2016). Since nonbenzodiazepine hypnotics, or “Z-drugs,” the most well-researched, moderately effective, and have fewer side effects than benzodiazepines, they are probably the first class of drugs that doctors typically provide to people who have insomnia. The effects on total sleep time vary, but each medication in this class will reduce sleep latency by about 20 minutes (Bragg et al., 2019).Melatonin and sedating Histamine-1-Receptor Antagonists (Doxylamine and Diphenhydramine) are two over-the-counter medications that are marketed for the treatment of insomnia, but there is insufficient evidence to support the use of these medications (Silber, 2005). According to data from observational studies, hypnotic medications may have major side effects like dementia and fractures. FDA product labels alert patients to potential adverse effects and cognitive and behavioural changes, including impaired driving and auto accidents (Qaseem et al., 2016).
4.4. Cognitive behavioural therapy for insomnia
Changes in behaviour (bad sleep habits, irregular sleep schedules), psychology (unrealistic expectations, worry, unhelpful beliefs), and physiology (mental and somatic tension, hyperarousal) are among the factors that CBT aims to address in order to address insomnia (Morin & Benca, 2012). Treating chronic insomnia with cognitive behavioural therapy for insomnia (CBT-I) is effective. This therapy focuses on thoughts and behaviours related to sleep and consists of multiple sessions and components (Mysliwiec et al., 2020). For patients, mobile applications like the Veterans Affairs' CBT-I coach offer a fresh and user-friendly addition to CBT-I. The CBT-I coach serves as a central location to monitor sleep patterns, offer techniques (like guided imagery and relaxation breathing), and promote positive reinforcement (Bragg et al., 2019). Overall, CBT-I is more cost-effective than pharmaceutical treatment. Pharmacologic treatments for insomnia are meant to be used temporarily, as stated on the FDA label, and patients are advised not to use these medications for prolonged periods of time (Qaseem et al., 2016).
Behavioural components include Counter arousal techniques and Relaxation Therapy, stimulus control (building a stronger link between the environment in which you sleep and your ability to sleep), sleep hygiene education, and Sleep Restriction Therapy (limiting the amount of time you spend in bed to sleep time, followed by a gradual increase in time in bed as sleep efficiency improves) (Mysliwiec et al., 2020).Overall, CBT-I is more cost-effective than pharmaceutical treatment. Pharmacologic treatments for insomnia are meant to be used temporarily, as stated on the FDA label, and patients are advised not to use these medications for prolonged periods of time (Qaseem et al., 2016).
4.5. Acute Insomnia
Three key ideas are important to consider when searching for “caseness,” or whether a person has experienced a condition that qualifies them as a “case,” or if they have not experienced an illness, disease, or disorder. The duration, frequency, and severity of the symptoms are among the concepts that centre on the presenting symptoms and their accompanying features. Furthermore, one must consider the circumstances surrounding the beginning of an illness, such as acute insomnia, when conceptualising the onset of the condition (i.e., triggering factors) (Ellis, Perlis, et al., 2012). Cortisol, the final hormone produced by the HPA axis, is a stress marker that is particularly relevant to the emergence of acute insomnia. The hypothalamus releases Corticotropin-Releasing Hormone (CRH) in reaction to perceived as risks during stressful situations. This, in turn, sets off the Anterior Pituitary Gland's release of Adrenocorticotropin Hormone (ACTH), which in turn sets off the adrenal cortex's release of cortisol. a few studies demonstrate distinct changes to cortisol and the Cortisol Awakening Response (CAR), which may suggest that insomnia disorder is characterised by elevated HPA axis activity. In particular, research has shown that individuals with insomnia have higher levels of cortisol in the morning, more CARs, and higher levels of cortisol in the 24-hour period than those without insomnia disorder. Even though the HPA axis is relevant to insomnia disorder, not much is currently known about how the HPA axis is active during the acute phase of insomnia (Elder et al., 2023).
A recent effort was undertaken to describe and conceptualize Acute Insomnia while taking into account the fundamental components of insomnia disease (as stated in the proposed DSM V nosology). The presence of a trigger and a numerical indicator of the degree of the sleep complaint—such as a Sleep Onset Latency or Wake After Sleep Onset of thirty minutes or more—were added to this definition (Ellis, Gehrman, et al., 2012).
4.5.1. Diagnosis
Medication, behavioural and psychiatric therapies, and a range of complementary and alternative therapies (such as yoga, acupuncture, and herbal remedies) are examples of specific insomnia therapies (Morin & Benca, 2011). In order to ascertain if an individual has met or surpassed a limit and may be categorized as a “case,” it is essential to consider three fundamental principles while searching for “caseness”—that is, the existence or nonexistence of a of a sickness, disease, or disorder. The duration, frequency, and severity of the symptoms are among the notions that centre on the presenting symptoms and their accompanying aspects. Furthermore, one must consider the conditions surrounding the beginning of an illness, such as acute insomnia, when conceptualizing the onset of the condition (i.e., triggering variables). The International Classification of Diseases (ICD-10), the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), and the International Classification of Sleep Disorders, Second Edition (ICSD-2) are the three diagnostic systems that are used in sleep research and practice to define “caseness.”. The DSM and ICD, two of these three diagnostic guides, classify insomnia types and subtypes using various criteria and employ a category multiaxial framework (Ellis, Gehrman, et al., 2012).
4.5.2. Treatment
4.5.2.1. International classification of diseases (ICD)
Based on the definition of nonorganic insomnia (NI) (F51.0), conclusions can be drawn under ICD-10. For a disorder to be considered non-infectious (NI), it must be present for a minimum of one month, The people should have sleep disturbances for a minimum of three nights out of every week (Ellis, Gehrman, et al., 2012). The classification of diseases, 10th edition (World Health Organisation, 1993) made a distinction between sleep disorders classified as organic and those classified as non-organic (Riemann et al., 2022).If you experience acute insomnia, It falls under the category of nonorganic insomnia that lasts shorter than a month. Given that both acute and chronic insomnia are described as nonorganic diseases, it stands to reason that both would require a non-biological cause. Regarding daytime consequences, even though the ICD requires attention to or awareness of them, there is no reason to believe that, in the acute form of the disorder, the person is or is not more focused on the insomnia's occurrence than the trigger (Ellis, Gehrman, et al., 2012).
It is noteworthy to mention that insomnia is likely more common to occur in co-morbid conditions with mental and physical disorders than it is to occur in isolation. The DSM-5, ICSD-3, and ICD-11 recognise this by allowing co-morbidity outright. it was also discovered that Cognitive-Behavioural Therapy for insomnia (CBT-I) improves quality of life and somatic/mental co-morbidities in addition to having a significant impact on sleep/insomnia complaints (Riemann et al., 2022). An individual's subjective complaint of inadequate sleep, combined with B¼ The six major criteria for a differential diagnosis are a reported inability to initiate, maintain, or experience early morning awakenings. Moreover, there must be reports of discomfort or impairment (C), for at least three nights per week (D), for at least three months (E), even though they have had enough opportunity to sleep (F). Like the ICD, the DSM-V does not have a specific diagnosis for acute insomnia (Ellis, Gehrman, et al., 2012).
4.5.3. Transient insomnia
Introduction: The symptoms of transient insomnia include trouble falling or staying asleep for a few days to a few weeks. Despite being a widespread ailment, transient insomnia is still largely unstudied, partly because research on the disorder is inherently challenging. According to research, treating and diagnosing temporary insomnia early on may delay the development of chronic sleep problems. Transient insomnia is thought to be one of the predisposing factors for the development of chronic insomnia, in addition to the possibility of immediate consequences (Roth et al., 2010).
Transient insomnia typically manifests as a condition that has persisted for a few days or weeks, albeit it may have returned in response to specific events. It might result from an abrupt shift in the surroundings, challenges brought on by adjustments to work or sleep schedules, or most commonly, an intense emotional crisis (Nicholson & Marks, 1983). In addition to chronic insomnia, many people also suffer with acute sleep disturbances on occasion, often known as transitory insomnia, and its detrimental implications. Numerous emotional and environmental variables, such as sudden stress, grief, schedule changes, travel, and stimulant usage, can cause transient sleeplessness. A complaint of several days to a few weeks is usually considered transient insomnia, whereas a complaint of at least three weeks is considered chronic insomnia (Rosenberg et al., 2005). The “first-night effect” was employed in this study to investigate the effectiveness of Eszopiclone in this model of Transient insomnia; this model has been confirmed in multiple research using healthy adult sleepers. This study's main goal was to use polysomnography (PSG) to compare the hypnotic efficacy of eszopiclone 3 and 3.5 mg to that of a placebo (Rosenberg et al., 2005).
Treatment: After receiving eszopiclone treatment, patients' PSG latency to persistent sleep was considerably shortened (all doses except 1 mg; P≤0.0001), their sleep efficiency increased (all doses; P≤0.02), and their wake time after sleep start decreased (all doses; P≤0.05). Furthermore, there were less awakenings in the patients (3 and 3.5 mg doses; P<0.005). The self-reported efficacy results were similar to PSG. Eszopiclone 3 and 3.5 mg significantly improved self-reported morning drowsiness scores when compared to placebo (P<0.05) (Rosenberg et al., 2005). After enrolling in the study, 565 participants were randomised to receive either a placebo (n = 282) or doxepin 6 mg (n = 283). In this model of transient insomnia, a single 6 mg dose of doxepin given to healthy volunteers was well tolerated and resulted in significant improvements in PSG-defined and patient-reported sleep onset, maintenance, and duration endpoints that lasted into the last hour (hour 8) of the night. Every hour of the night saw a significant improvement in LPS, LSO, WASO, TST, sTST, and SE, with all p-values being extremely significant (p ≽ 0.0003) (Roth et al., 2010).
5. NARCOLEPSY
Clinicians currently distinguish between two types of Narcolepsy, with the common feature being chronic daytime sleepiness. Cataplexy and a significant reduction in orexigenic neurons, which are responsible for the release of orexin-A and orexin-B neuropeptides, are the hallmarks of type 1 narcolepsy. Cataplexy is not seen in type 2 narcolepsy, and orexin concentrations do not change (Nepovimova et al., 2019). Even though narcolepsy is common, it takes an average of five to fifteen years between the onset of symptoms and the diagnosis. Because many clinicians are not familiar with this disorder, up to half of all affected individuals may go undiagnosed (Scammell, 2015).
5.1. Pathophysiology
The pathophysiology and aetiology of narcolepsy were clarified by the ground-breaking discovery of the Neuropeptide Hypocretin/orexin, the lack of which is currently thought to be responsible for the majority of Narcolepsy symptoms (Nepovimova et al., 2019). Major pathophysiology appears to be the loss of up to 95% of hypocretin-producing neurons in the lateral hypothalamus, which causes low CSF hcrt-1 levels (Type I narcolepsy) (Abad, 2017). Over 85% of individuals with type 1 narcolepsy are associated with a particular human leukocyte antigen (HLA) allele, HLA DQB1*0602. B cells, dendritic cells, and activated T cells all express HLA class II molecules (Nepovimova et al., 2019). HLA DQB1*06:02 is strongly linked to narcolepsy, and polymorphisms in the T-cell-receptor-α (TCRA) locus on chromosome 14, TNFSF4 (also known as OX40L), Cathepsin H (CTSH), the purinergic receptor P2RY11, the DNA methyltransferase DNMT1, and carnitine palmitoyl transferase (CPT1B) have been found in genome-wide association studies (Abad & Guilleminault, 2017). Sleep paralysis, hypnagogic hallucinations, and cataplexy, among other REM sleep-related abnormalities, are likely caused by a particular combination of pathophysiologic conditions in the brain (Mitler et al., 1987).
It is believed that REM sleep dysregulation symptoms arise from the sporadic activation of REM sleep-promoting neurons during wakefulness, which causes REM sleep manifestations—like cataplexy—to intrude into wakefulness (Thorpy & Bogan, 2020). It has been demonstrated that mice devoid of B and T cells are especially vulnerable to influenza A (H1N1) viral infection, and that autoreactive cytotoxic CD8+ T cells injected into transgenic mice expressing the influenza virus protein hemagglutinin in the hypocretin cells resulted in the destruction of hypocretin neurons (Dauvilliers & Barateau, 2017). This spike in new cases indicates that narcolepsy risk is strongly increased by DQB1*06:02, young age, and specific immune stimuli (Scammell, 2015). Two types of narcolepsies are now recognised by clinicians. People with both disorders exhibit persistent daytime sleepiness and score well on the multiple sleep latency test (Scammell, 2015). Narcolepsy type 1 is typified by cataplexy and very low levels of orexin-A in the cerebrospinal fluid (Scammell, 2015). It is caused by a selective loss of a small population of neurons in the lateral hypothalamus that synthesise hypocretin neuropeptides (Dauvilliers & Barateau, 2017). Cataplexy is absent in type 2 narcolepsy patients, and their orexin-A levels are normal (Scammell, 2015). But have MSLT or PSG + MSLT confirmation of EDS, and the CSF hcrt-1 concentration is not measured, or the CSF hcrt-1 is greater than 110 pg/mL or greater than 1/3 of the mean values obtained in normal subjects (Abad & Guilleminault, 2017) (Figure 6)
5.2. Diagnosis
Narcolepsy can be distinguished from other forms of excessive somnolence by supplementary symptoms. The hypnagogic hallucinations, sleep attacks, cataplexy, and sleep paralysis that comprise the narcoleptic tetrad are among them (Mitler et al., 1987). In order to diagnose each patient and meet the international diagnostic standards of the International Classification of Sleep Disorders (ICSD-32014), overnight PSG and MLT studies were conducted (Abenza-Abildua et al., 2023). In ICSD-3, narcolepsy type 1 is defined as excessive daytime sleepiness lasting longer than three months, accompanied by either cataplexy (a mean sleep latency of eight minutes or less on the multiple sleep latency test.) or a highly specific biological measure called hypocretin-1, with a level in the CSF of 110 pg/mL or less (Dauvilliers & Barateau, 2017). In the US, type 1 is present in 0.02%–0.18% of cases. Although the exact point prevalence of type 2 disease is unknown, 20.5/10,000 has been proposed (Abad & Guilleminault, 2017).
5.3. Treatment
Treatment based on OXR agonists, gene therapy, Orexin Cell Transplantation, or even just substituting Orexin. Orexin delivery methods include intravenous (IV), intracisternal, and intranasal routes (Nepovimova et al., 2019). Orexin replacement therapy should be a successful tactic for re-establishing orexin signalling because narcolepsy type 1 is typified by the loss of orexin neurons. Exogenous orexin peptides, pro-drug precursors, or small-molecule agonists may accomplish this (Nepovimova et al., 2019). Potential therapeutic delivery to the central nervous system (CNS) is typically restricted by the Blood-Brain Barrier's (BBB) permeability. After intravenous injection measured the rate at which 125I-labeled orexin-A and orexin-B entered the brains of albino ICR mice, localising them in the brain parenchyma or binding to BBB endothelial cells. According to their suggestion, orexin-B is a small lipophilic peptide that metabolises quickly in the bloodstream. It was demonstrated that orexin-A is extremely lipophilic and enters mice's brains quickly through simple diffusion (Nepovimova et al., 2019).
Specifically, the inability of orexin peptides to penetrate the blood brain barrier in meaningful amounts has made drug delivery challenging. Even though research on animals revealed that orexin-A administered intravenously raised drug concentrations in brain tissue and lessened the effects of sleep deprivation (Thorpy & Bogan, 2020). All 51 patients had taken the prescribed medications (methylphenidate, modafinil) to treat their drowsiness. Just four (22.22%) of the eighteen anxiety syndrome patients were able to take them on time and at low doses because their symptoms were getting worse (Abenza-Abildua et al., 2023).Sodium Oxybate is the only drug accepted for treating adult cataplexy and sleepiness together. The appropriate course of Anti cataplexic treatment should be determined by the severity of the symptom; mild cataplexy often improves with increased alertness after wake-promoting therapies are started (Dauvilliers & Barateau, 2017).
6. RESTLESS LEG SYNDROME
6.1. Introduction
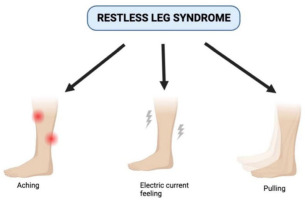
An overwhelming need to move one's legs and restlessness, frequently accompanied by unpleasant sensations is called as restless leg syndrome (Gossard et al., 2021). It has been stated that restless legs syndrome is either a symptomatic disorder with no known cause or an idiopathic disorder that is frequently linked to end-stage renal disease, pregnancy, and iron deficiency (Trenkwalder et al., 2005). The clinical characteristics of the lower extremities, such as paraesthesia, urticaria, and itching in a family member, were recognised by Mussio-Fournier and Rawak (Tuna Oran et al., 2021) and also by uncomfortable leg sensations that are usually felt during rest before sleep sets in and are eased with movement. RLS usually starts in the thighs or calves and progresses clinically to other lower limb areas, including the foot (Yeh et al., 2016). In addition, persistent sleep loss and trouble falling asleep are frequent and upsetting symptoms of RLS (Maiolino et al., 2021). RLS that is clinically severe affects 2 to 3 percent of people in Europe and America. It severely disrupts sleep, quality of life, and productivity during the day and frequently necessitates years, if not lifetime, of treatment (Allen, 2014).The idea that RLS also carries a higher risk of adverse cardiovascular events has been reinforced by recent research (Maiolino et al., 2021). There is no clear pathogenesis for RLS. Currently, the disorder is divided into two categories: idiopathic (familial or sporadic) and secondary (related to pregnancy, chronic kidney disease, Parkinson's disease, or conditions that cause iron deficiency or changes in iron metabolism) (Lebrato Hernández et al., 2022) (Figure 7).
6.2. Epidemiology
The prevalence of RLS varies significantly by region; it is highest in populations in Europe (1%–8% in Asian nations, 5%–12% in African nations, and lowest in Asian countries (less than 1%), where the fewest studies have been conducted. RLS affects women more frequently than men, with parity playing a key role (Trotti, 2017).The problems this study raises would be especially significant in epidemiology studies where non-clinicians conduct telephone surveys with members of the public, with the goal of including only patients with primary RLS (Yeh et al., 2016). In fact, the main problem with RLS epidemiological research is that RLS is only identified by the patient's self-reported symptoms. Whether or not objective criteria are eventually useful in diagnosing RLS depends on how well-understood the patient's symptoms are and how forthcoming the patient is with the researcher, as the sensations are subjective to the patient. As previous international studies have noted, the true prevalence rate of restless legs syndrome may actually be underestimated due to a variety of factors, including the belief that restless legs are a minor ailment that doesn't require medical attention, the fear that affected individuals will be shunned in some cultures, and the absence of symptoms when testing a patient while they are awake (Yeh et al., 2016).
6.3. Pathophysiology
RLS may exacerbate mood by interfering with sleep. Mood symptoms can benefit, if only slightly, from RLS treatment. In 9% of patients, antidepressants also induce or exacerbate RLS. With Mirtazapine (28%), this effect is more noticeable than with duloxetine (5%), and it is less noticeable with citalopram (Trotti, 2017). The majority of reports of RLS caused by antidepressants have included serotonergic medications like sertraline, paroxetine, and fluoxetine. Mirtazapine, the first noradrenergic and specific serotonergic antidepressant (NaSSA) with presynaptic antagonistic, 5-HT receptor stimulating, and 5-HT2/5-HT3 receptor-blocking properties, has been linked in a number of case reports to RLS. The most likely second-generation antidepressant to cause RLS is probably mirtazapine. Furthermore, the longest axons of the dopaminergic Diencephalospinal tract project to the dorsal horn of the spinal cord, which has been hypothesised to be a component of the pathological process for RLS. When compared to non-RLS patients, RLS patients also exhibit abnormal activation of the gastrocnemius muscles, which are located in the upper calf, during walking. This finding raises the possibility that patients with RLS may have compromised supraspinal dopaminergic control over the muscle (Yeh et al., 2016).
One possible mechanism through which CNS iron levels influence the pathophysiology of RLS is by means of hypoxic-state pathway activation. The RLS patient's microvasculature showed increased levels of vascular endothelial growth factor (VEGF), hypoxia-inducible factor 2-alpha, and substantia nigra neurons on higher levels (Gossard et al., 2021). They also have been found to have iron deficiency quite frequently, and brain iron deficiency may play a significant role in the pathophysiology of RLS (Earley, 2003) Both Ekbom and Nordlander examined how iron functions in RLS during the initial phases of the illness. Numerous imaging studies have demonstrated a robust correlation between RLS and iron metabolism, especially in the brain (Gossard et al., 2021).
In addition to the spinal component, Lanza et al. state that a number of mechanisms, such as diminished central inhibition and anomalies in peripheral nerve function, may be involved in the pathophysiology of RLS. Dopamine and iron are closely related; a prominent theory suggests that low cellular iron modifies some aspects of the dopaminergic system either directly or indirectly. It is more intricate than just the proportion of these molecules, though. It is reasonable to assume that brain dopamine levels should be low in RLS patients because dopamine agonists alleviate the symptoms of RLS. Studies conducted thus far, however, have not revealed this to be the case (Gossard et al., 2021).
6.4. Diagnosis
The desire to extend one's limbs, notably one's leg, is the primary indicator of RLS diagnosis. Unpleasant and uncomfortable sensations may or may not accompany this urge (Yeh et al., 2016). Subjective sleep quality was impacted in the current study, and participants with recently diagnosed severe degree RLS experienced more sleep disturbances. The degree of RLS was found to positively and significantly correlate with a delay in the onset of sleep in a study conducted in Bangalore, India (Joseph et al., 2022). The clinical Hopkins telephone diagnostic interview was utilised to confirm the diagnosis. Symptoms occurring at least fifteen times within the month before the screening, symptoms that started at least half a year before to screening, and symptoms that mostly happened at night were all considered eligibility requirements. A one-week trial of placebo was also required, with the participant's score on the IRLS Study Group Rating Scale must be at least 15 at the beginning and end. Higher scores on the IRLS scale indicate more severe symptoms: variations in scores greater than three are considered clinically significant. The scale has a range of 0 to 40 (Allen et al., 2014).
Assessments of peripheral iron stores (ferritin, transferrin saturation) should be made both during the initial diagnosis of RLS and later during long-term care (Gossard et al., 2021). Since iron deficiency is often linked to restless legs syndrome, serum ferritin concentration should be tested in all patients (Trenkwalder et al., 2005). Research has also revealed that children with RLS diagnoses have greater rates of ADHD and are more likely to have RLS-diagnosed parents (Yeh et al., 2012).Compared to the general population, people with poor mental and physical health experience RLS more frequently. The risk of developing RLS is also highest in the elderly (Yeh et al., 2012).Most researchers added to their inclusion criteria a minimal IRLSRS score at baseline, generally including participants with a “moderate to severe” condition (Guay et al., 2020).
Diagnosis tests include (Guay et al., 2020) (Figure 8)
Most of the time, cramps can be easily differentiated from RLS because they are characterised by a distinct knotting of a muscle, whereas the latter causes excruciating localised muscle pain. After a prolonged period of sitting, a patient may experience paraesthesia's in one or both feet. These can be relieved by shifting positions or crossing and uncrossing the legs 43q (Earley, 2003).
6.5. Treatment
For people who have iron deficiency, iron supplements are advised (Marshall et al., 2019).
It has long been known that iron supplementation is beneficial for RLS patients. It's also important to identify and address the source of the iron deficiency. After three months, ferritin levels should be checked while starting first-line oral supplementation. Intravenous injection is an option to consider if oral iron supplementation proves to be ineffective (Limousin et al., 2018). RLS nonpharmacologic treatment may be beneficial when used as adjunctive or monotherapy. Aerobic exercise and lower body resistance reduce the severity of RLS (Trotti, 2017). Based on the vascular theory of the disease, lifestyle interventions that support improved circulation and cardiovascular health as well as overall health are appropriate for treating RLS (Bega & Malkani, 2016). The fact sheet offers advice on cutting back on alcohol, cigarettes, and caffeine in addition to maintaining regular sleep schedules and engaging in moderate exercise on a regular basis (Bega & Malkani, 2016).Those suffering from restless legs syndrome report augmentation because of dopaminergic treatment. The terms “augmentation,” “increase in severity of symptoms,” and “involvement of other body parts” refer to the early onset of symptoms during the day (Trenkwalder et al., 2005). Table 3 gives a brief idea about the medications used for treating sleep disorders and are explained below.
Levodopa
Levodopa has been shown in numerous placebo-controlled randomised trials to be effective in treating RLS (Limousin et al., 2018) levodopa was found to be useful in treating nocturnal symptoms of restless legs syndrome as well as improving both the subjective and objective quality of sleep-in patients with idiopathic and uraemic disease. For the treatment of the syndrome, Levodopa plus Benserazide has been authorised for a number of years in Germany, Switzerland, and Austria (Trenkwalder et al., 2005).
Dopamine agonists
The ergot-dopamine agonists Bromocriptine, Pergolide, and Cabergoline, and the non-ergot dopamine agonists pramipexole, ropinirole, and rotigotine have all been shown to be effective in double-blind studies. The first double-blind randomised crossover study of a dopamine agonist used 7.5 mg bromocriptine at bedtime with five out of six patients having partial subjective improvement in restlessness and paraesthesia (Trenkwalder et al., 2005). A dopaminergic receptor D1, D2, and D3 agonist, pramipexole has a greater affinity for D3 receptors. Its half-life is 8–12 hours, and it takes 1–2 hours for it to start working. Eight level 1A studies have shown how effective it is on RLS both short- and mid-term (6 months) (Limousin et al., 2018).
Clonidine
Despite not having FDA approval, clonidine is a commonly used paediatric sleep aid due to its quick and easy absorption by kids and good tolerance. Alpha-2-adrenergics have occasionally been administered in conjunction with iron supplements. Adult RLS sensory symptoms have been successfully treated with clonidine in one randomised, double-blind, placebo-controlled trial without any negative side effects (L. DelRosso & Bruni, 2019).
Opioids
Opioids were empirically used for many years as a substitute RLS treatment (Limousin et al., 2018), treats RLS via their action on dopaminergic receptors (L. DelRosso & Bruni, 2019). Opioids are considered a therapy option of last resort. Opioids are first-choice medication for patients who are intolerant to dopaminergic agents (Trenkwalder et al., 2005). First-line use of level I opioids, primarily tramadol (Topalgic1), is permissible. There are two dosage forms of Tramadol: a 250 mg/5 mL oral solution and 50 mg capsules. There are pills with dosages of 100 mg, 150 mg, and 200 mg for extended-release forms (Limousin et al., 2018).
Clonazepam
Research using Polysomnography has revealed that clonazepam helps RLS patients sleep better and experience fewer arousals, but it does not effectively lessen the motor and sensory abnormalities linked to the condition (L. DelRosso & Bruni, 2019). It is not advised to use it as the RLS's first line. It can be applied on an as-needed basis (during an exacerbation of RLS, for example) (Limousin et al., 2018). Some common symptoms of sleep disorders are listed in Table 5.
7. CONCLUSION
Obstructive Sleep Apnoea, pharyngeal imaging is performed during waking will help us to find the pathophysiology in patients. Men are more likely than women to have OSA in middle-aged and elderly individuals over the age of sixty which may lead to cardiovascular mortality when they are diagnosed with OSA. A logical approach for treatment of OSA includes lifestyle modification, CPAP and in severe cases surgery. CSA is far less common than OSA. At high altitudes, CSA usually consists of two to three breaths interspersed with Apnoea between each burst. CPAP is used in treatment of CSA. Moreover, insomnia, based on PHQ-9 to a patient she scored 14 out of 27 which indicated moderate depression. Treatment includes pharmacologic therapy along with benzodiazepines for Chronic Insomnia, CBT-1 for Acute Insomnia and eszopiclone, Doxepin for Transient Insomnia. Additionally, narcolepsy, studies done using electrographic monitoring have showed inability to sustain periods of sleep. HLA is linked to more than 85% of cases of type 1 narcolepsy. Treatment includes Gene therapy and Orexin cell Transplantation. Therefore, the clinical Hopkins telephone diagnostic interview was used in the confirmation of the Diagnosis of RLS. Iron supplements are prescribed for the RLS patients along with drugs like Levodopa, Dopamine agonists, Opioids, Clonidine and Clonazepam.
Acknowledgement
We would like to thank CHRIST (Deemed to be University) for providing the necessary support and guidance to carry out this review.
Author contributions
Credit statements: conceptualization: M.P.; Methodology: G.M.; Validation, Formal analysis and Investigation: S.K.; K.J.; M.P.: G.M.; Writing – Original Draft: S.K.; K.J.; Writing – Review and Editing: S.K.; K.J.; M.P.; Visualization: S.K.; K.J.; Supervision: M.P.; G.M.; guiding - Final drafting: G.M.