Introduction
Burns refer to injuries affecting the skin or other organic tissues, resulting from exposure to high temperatures, electromagnetic waves, electrical currents, mechanical friction, or hazardous substances. Thermal burns are the most common type, often resulting from exposure to hot liquids, hot solid objects, or flames. According to World Health Organization (WHO) data, burns are a global concern, causing approximately 180,000 deaths on an annual basis (World Health Organization, 2018; Yakupu et al., 2022). A significant proportion of burn injuries—over 90%—are concentrated in low- and middle-income regions such as Africa and Southeast Asia. In contrast, high-income countries experienced a decrease in death rates from burns (Yakupu et al., 2022). Data from Hasan Sadikin Bandung General Hospital in Indonesia from 2015 to 2017 showed that among 373 burn injury patients, a total of 100 patients sustained extensive burn trauma, and 55% of those patients experienced sepsis (Soedjana et al., 2020).
According to the American Burn Association, burn classification is done by evaluating the appearance of the burn area, blanching with pressure, as well as the pain and sensation experienced by the patient. Superficial burns, or first-degree burns, involve the epidermis alone and are marked by a dry, pink to red area with no blisters. The pain experienced by the patient is moderate and can heal without scarring within 5 to 10 days. Superficial second-degree burns impact the upper dermis, displaying a moist, red surface that temporarily whitens under pressure and commonly forms blisters. The pain experienced by the patient is very severe. Healing can occur within 3 weeks with minimal scarring. Second–degree burns (deep partial) involve a deeper dermis and are characterized by a dry, white or yellow burn area that does not blanch with pressure. The pain experienced by the patient is minimal due to decreased sensation. Complete recovery may occur, ranging from three to eight weeks, though scarring is likely. Full-depth burns (third-degree burns) involve the full thickness and structure of the skin and are characterized by a hard, dry burn area that is white or brownish–black and does not blanch with pressure. The pain experienced by the patient is minimal due to decreased sensation. Healing takes more than 8 weeks and may heal with contracture. Severe fourth-degree thermal injuries penetrate beyond the skin to affect muscles and bones, often presenting as a blackened burn area with sections of missing tissue. The patient feels little to no pain or sensation (Jeschke et al., 2020; McCann et al., 2022; Warby & Maani, 2023).
A burn injury results in three key zones: the innermost coagulation zone, where irreversible damage occurs; the stasis or ischemia zone, which contains tissue with the potential for recovery; and the outer hyperemia zone, which experiences increased inflammation and vasodilation (Bourdon et al., 2017; Żwierełło et al., 2023). Cellular injury in each zone varies and may involve direct autophagy, delayed apoptosis, and reversible oxidative stress. Burns also trigger an inflammatory and stress response in the body several hours after injury. This can be characterized by the release of cytokines and stress hormones (catecholamines and cortisol) that cause distributive shock. This shock results from disruptions in tissue perfusion and oxygen distribution due to capillary leakage, contributing to tissue edema and organ dysfunction. The post-burn response transitions from an initial hypometabolic phase to a hypermetabolic state that may extend for as long as 36 months. In response to stress, hormones elevate blood pressure and insulin resistance while promoting the catabolism of glucose stores, body proteins, and fat deposits, leading to greater energy consumption, increased core body heat, protein depletion, and the synthesis of acute-phase proteins. This causes organ catabolism, dysfunction, and potential death. Additionally, burns significantly impact the immune system, activating immune cells and triggering inflammatory pathways. However, crucial immune functions such as macrophage antigen presentation and pathogen killing by neutrophils are impaired. Impaired Interleukin-2 (IL-2) secretion and reduced T cell proliferation disrupt the effectiveness of the adaptive immune response. This immune dysregulation increases susceptibility to infection. Severe burn patients face a heightened likelihood of infections, which may progress to organ failure and fatal outcomes (Burgess et al., 2022; Markiewicz-Gospodarek et al., 2022; Rae et al., 2016).
The body's reaction to a burn injury depends on various factors. These factors include burn severity—measured by depth and size—the cause of the injury, and associated complications such as inhalation injuries, contact with hazardous materials, and other compounding injuries. Additionally, patient-related elements like biological age, underlying health conditions, substance use, and the time taken to seek medical attention can significantly affect recovery (Jeschke et al., 2020). Even with the presence of multiple topical treatments for burn wounds, there is still an unmet need for effective drugs, as most available products prioritize antimicrobial effects over actual wound healing. Natural remedies from plants and herbs are an alternative topical burn therapy (Hossain et al., 2020; Saeidinia et al., 2017).
Renowned for its wound-healing properties, Centella asiatica—commonly known as gotu kola—has been a staple in traditional medicine for a long time. Packed with phytochemical compounds such as madecassoside, asiaticoside, asiatic, and madecassic acid, this plant extract offers antioxidant and anti-inflammatory effects and supports collagen formation. According to research, Centella asiatica contributes to faster wound recovery by stimulating fibroblast proliferation and collagen buildup while minimizing scar tissue formation (Park, 2021). However, research regarding the potential of Centella asiatica in burn wounds is still limited.
The objective of this literature review is to investigate the role of Centella asiatica in the healing of burn wounds. This review seeks to provide an in-depth overview of Centella asiatica's contribution to wound healing by analyzing current research. The primary focus will be on its mode of action, its effectiveness as demonstrated in clinical and preclinical studies, and its potential use in modern burn care strategies. Through this analysis, the review aspires to highlight the significance of Centella asiatica as a promising candidate for enhancing burn wound care.
The process of healing burns and their treatment
The recovery of burn wounds follows four primary stages: coagulation, immune response activation, tissue regeneration, and repair. Following an injury, the initial phase commences, marked by constriction of blood vessels, platelet response, and clot development. During this process, growth and clotting factors, including platelet-derived growth factor (PDGF), epidermal growth factor (EGF), and transforming growth factor-beta (TGF-β), are released by platelets, keratinocytes, macrophages, and fibroblasts, ultimately forming a fibrin clot at the wound site. The fibrin clot serves as a provisional scaffold for the subsequent phases of healing. Within 24 hours, the immune activation begins, driven by local vasodilation that attracts monocytes and neutrophils to the wound. This phase, lasting weeks to months, involves the emission of inflammatory mediators, chemokines like interleukin-1 (IL-1), interleukin-8 (IL-8), and tumor necrosis factor (TNF), as well as growth factors such as TGF-β, insulin-like growth factor (IGF), and vascular endothelial growth factor (VEGF). Neutrophils and macrophages contribute to wound healing by eliminating cellular waste and infectious organisms. During the tissue regeneration phase, fibroblasts and keratinocytes are stimulated to replace the temporary scaffold with a connective tissue matrix, supporting wound tissue development, capillary formation, and skin regeneration. Keratinocytes are crucial in closing the wound surface and restoring blood flow. Growth factors like VEGF, hepatocyte growth factor (HGF), and fibroblast growth factors (FGFs) stimulate endothelial cells for new blood vessel formation. Resident fibroblasts convert into myofibroblasts, contributing to the deposition of extracellular matrix (ECM). In the final repair phase, granulation tissue undergoes maturation, and the extracellular matrix (ECM) is reorganized through the action of growth factors, matrix metalloproteinases (MMPs), and their inhibitors (TIMPs), leading to wound contraction and reinforcement (Abazari et al., 2022; Korkmaz et al., 2023; Oryan et al., 2017; Rose & Chan, 2016).
In emergency burn care, the Advanced Trauma Life Support (ATLS) framework is applied, with an emphasis on stabilizing airway, breathing, and circulation (ABC). During the primary assessment, medical personnel identify breathing difficulties and inhalation injuries, evaluate cardiovascular health for signs of shock, detect concurrent injuries, and assess the burn's severity and extent using total body surface area (TBSA) calculations. Acute care stabilization begins upon arrival and continues until transfers to the intensive care unit. Key actions to stabilize severely burned patients include managing the airway, providing respiratory support as needed, administering fluid resuscitation, ensuring cardiovascular stability, managing pain, and efficiently addressing burn wounds (Rowan et al., 2015; Vigani & Culler, 2017).
Burn wound management includes hydrotherapy and wound cleansing, eschar removal, and the use of topical antibiotics. Immediate hydrotherapy for burn patients can offer several benefits, including reducing the formation of the zone of coagulation, minimizing edema, speeding up re-epithelialization, and enhancing pain control. It is recommended to use cool water or gauze soaked in saline at 12°C (54°F) for 15 – 30 minutes. Refraining from using ice or cold water is critical to avoid vasoconstriction, the onset of hypothermia, and further injury complications. To avoid hypothermia during burn cooling, it is advisable to monitor rectal temperature, particularly in patients with burns affecting more than 15% of the total body surface area. Core body temperature stability can be supported through the administration of pre-warmed intravenous fluids, protective thermal coverings, and the initial covering of affected skin areas. Irrigation of burn wounds can help remove residual debris, and adding mineral oil to hydrotherapy can aid in removing tar. Disinfectants should be avoided, saline solution or non-irritating soap and water are preferable for wound decontamination (Rowan et al., 2015; Vigani & Culler, 2017).
Eschar is a rigid area that forms at the site of superficial and deep burn injuries. It can interfere with accurate burn classification and cause pain by pulling on damaged skin when the patient moves. Circumferential burn injuries with eschar can restrict respiratory movements and cause impaired perfusion in the limbs. Escharotomy is a potential intervention to alleviate compromised distal circulation in circumferential limb burns with eschar. Early eschar removal is recommended to prevent infection and facilitate direct application of medication to the wound, thus enhancing medication penetration (Rowan et al., 2015; Vigani & Culler, 2017).
Historically, silver sulfadiazine cream has been the preferred choice for topical burn therapy, primarily for its antibacterial benefits. However, the treatment has some shortcomings, including delayed healing characterized by slow epithelialization, impaired wound contraction, black scar development, limited penetration, hypersensitivity, and potential toxicity. Antimicrobial burn creams and solutions such as mafenide acetate and silver nitrate are associated with side effects, including tenderness and pain at the burn site, delayed recovery process, electrolyte abnormalities, and the chance of methemoglobinemia (Burgess et al., 2022; Markiewicz-Gospodarek et al., 2022). As a result, natural treatments from plants and herbs have become an alternative to topical burn therapy. This option is considered more accessible, cost-effective, widely usable, and less likely to be rejected, and it can accelerate the burn healing process (Hossain et al., 2020; Saeidinia et al., 2017).
Potential role of Centella asiatica in burn wound healing
Centella asiatica is a valuable botanical known for its therapeutic applications. It typically flourishes in the humid environments of tropical regions. This medicinal herb has been employed for generations to treat various health issues, with a strong presence in traditional practices of Asia and the Middle East. This plant has leaves shaped like a scoop or spade with wavy edges and grows on long stems that gather at the nodes of the stem. Extracts and active compounds from Centella asiatica are key components in various cosmetic and herbal preparations worldwide. Recognized globally by the names gotu kola and Indian pennywort, this plant has certain wound-healing properties, including for ulcerative skin conditions and burns. Additionally, Centella asiatica extract has been used to treat lupus, scleroderma, leprosy, and vascular diseases (Centella Asiatica (L.) Urb. | Plants of the World Online | Kew Science, n.d.; Gray et al., 2018; Sun et al., 2020).
The key active components of Centella asiatica include triterpenoid saponins (plant-based glycosides), triterpenoid genins (sapogenins), essential oils (volatile oils), flavonoids (polyphenolic compounds), phytosterols (plant sterols), and complementary active substances. Among these, the most important active components are triterpenoid saponins, which include madecassoside, asiaticoside, madecassic and asiatic acid. Collagen, a crucial protein in burn wound healing, is stimulated by triterpenoid saponins (plant-based glycosides) to aid in tissue repair (Gray et al., 2018; Sun et al., 2020).
Centella asiatica is known for its diverse pharmacodynamic actions, including wound repair, anti-inflammatory effects, and protection against microbial and fungal infections. It demonstrates remarkable efficacy in treating burns, infected wounds, and hypertrophic scars. By fostering angiogenesis, type I collagen formation, and speeding up epithelialization, it plays an integral role in accelerating the wound healing process. Its inflammation-modulating effects are significant even at small quantities and show increased effectiveness with larger doses. Additionally, Centella asiatica exhibits antibacterial and antifungal activities, making this medicinal plant widely used due to its lower risk of contamination. Centella asiatica oil has been found to exhibit antibacterial properties effective against bacterial strains of both gram-positive and gram-negative types. Furthermore, ethanol extract from Centella asiatica demonstrates strong antifungal activity (Hossain et al., 2020; Park, 2021; Saeidinia et al., 2017).
A clinical study of one percent Centella asiatica cream for chronic wounds showed promising results in accelerating wound healing. Asiaticoside extracted from Centella asiatica is known to enhance hydroxyproline, collagen, wound tightening, and the rate of skin layer regeneration. Asiaticoside aids in wound healing by stimulating fibroblast growth and extracellular matrix formation. It facilitates wound healing by boosting collagen synthesis and promoting neovascularization. The phosphorylation of Smad 2 and Smad 3 triggers type I collagen production in human dermal fibroblast. Previous research indicates that asiaticoside activates transforming growth factor-beta (TGF-β) receptor I kinase, which further facilitates collagen formation (Diniz et al., 2023; Lv et al., 2018).
Meanwhile, madecassoside actively contributes to enhancing burn wound healing by encouraging blood vessel growth, strengthening free radical defense, and facilitating collagen production. Histopathological studies have shown that madecassoside can reduce inflammatory cell infiltration and improve epithelialization through dermal fibroblast proliferation. When administered at a rate of 1 mg/kgBW and 2 mg/kgBW, this compound has been proven to reduce nitric oxide and malondialdehyde levels in burned tissue. Additionally, madecassoside also increases reduced glutathione and hydroxyproline, which are indicators of collagen synthesis in burn wounds. This contributes to necessary fibroblast activation and production of collagen fiber for successful burn wound healing. Various growth factors such as fibroblast growth factors (FGF), endothelial growth factors (EGF), and vascular endothelial growth factor (VEGF) also aid in the recovery of tissue function (Fernenda et al., 2023; Park, 2021).
Asiatic acid induces the expression of hyaladherin TNFAIP6, which aids in extracellular matrix formation in fibroblast cells and regulates metalloproteinase activity by maintaining the balance between MMP/TIMP, thus enhancing collagen synthesis. In experiments with mouse models, orally administered Centella asiatica has been shown to help speed up recovery from burn injuries by encouraging the development of new capillaries, fibroblast replication, and collagen biosynthesis, in tandem with narrowing of the wound. A separate study indicated that all extracts derived from Centella asiatica can help heal burn wounds. This suggests that the plant's diverse range of components work synergistically to promote wound closure and cellular repair (Diniz et al., 2023; Lv et al., 2018).
Research has reported various pharmacological activities of Centella asiatica; hence, the number of studies over the last 10 years regarding the potential of Centella asiatica in burn wound closure remains limited. Research on Centella asiatica's potential role in burn wound healing has resulted in 6 articles, as summarized in Table 1 and Table 2.
Table 1
| In vivo | |||
|---|---|---|---|
| No. | Researcher, year | Research methods | Research results |
| 1 | (Bardaa et al., 2016) | Administration of "Cytol Centella," a synthetic emulsion medication with active ingredients based on titrated natural Centella asiatica extract, at a dose of 0.13 mg/mm2 using sterilized dressings every 2 days in adult male Wistar rats with second – degree burns (deep dermal partial thickness). | |
| 2 | (Hou et al., 2016) | Topical application of the test compounds asiaticoside (AE) and madecassoside (MA) at a dose of 500 μl once daily for 14 days on male Sprague – Dawley rats with second – degree (partial thickness) skin burns. | |
| 3 | (Mayefis et al., 2016) | Topical application of single Centella asiatica extract at a concentration of 2% and a combination of Centella asiatica extract with papaya latex extract at a dose of 0.1 grams once daily for 10 days on male white rats with skin burns. | |
| 4 | (Armadany et al., 2023) | Topical application of single ethyl acetate extract of Centella asiatica at a concentration of 10% and a combination of ethyl acetate extract of Centella asiatica with virgin coconut oil twice daily for 21 days on male mice (Mus musculus) with skin burns. | |
Table 2
| Clinical trials | |||
|---|---|---|---|
| No. | Researcher, year | Research methods | Research results |
| 1 | (Muangman et al., 2016) | Randomized, double-blind controlled trial Patients with second – degree burns covering 20% or more of their total body surface area and aged between 18 and 60 years (n = 35) The burn wound area was treated and dressings were changed with polyester gauze coated with a mixture of 2.5% aloe vera extract and 5% gotu kola leaf extract every 3 days until complete healing (21 days). |
|
| 2 | (Saeidinia et al., 2017) | Randomized, double-blind controlled trial Patients with second-degree burns on the extremities, covering less than 10% of their total body surface area, and aged between 14 and 60 years (n = 60). Topical application of 3% Centiderm ointment, a derivative of Centella asiatica, was applied in adjusted amounts once daily until complete healing (25 days). |
|
A study conducted by Bardaa et al. on "Cytol Centella," a synthetic emulsion medication derived from natural Centella asiatica extract, demonstrated clinically significant reductions in burn wound size and increased percentage of wound contractions. The experiment included 24 adult male Wistar rats with deep dermal partial thickness skin burns on the back measuring 3.8 cm2. The rats were treated with "Cytol Centella" at a dose of 0.13 mg/mm2 using sterile dressings every 2 days from the day of burn induction until the negative control group achieved complete healing, which was 33 days. Measurements of burn wound size and wound contraction percentage were taken every 2 days using transparent paper. Histopathological examination with hematoxylin – eosin staining was performed to evaluate epidermal epithelial regeneration on the burn wound. Additionally, histomorphometric examination was also conducted to measure skin tissue regeneration structures, such as blood vessels, collagen, and inflammatory cells. The data revealed a substantial reduction in burn wound area, along with an increased percentage of wound contractions on days 9, 17, 25, and 33. Biopsy revealed regeneration in the epidermal epithelium with an augmentation of vascular network and collagen fibers, as well as a decrease in the volume of inflammatory cells. Expedited wound shrinking and restoration of skin epithelium during burn healing demonstrate that "Cytol Centella" exerts anti-inflammatory effects while stimulating fibroblast growth and collagen biosynthesis types I and III (Bardaa et al., 2016).
The use of active triterpenoid compounds from Centella asiatica has been observed to elevate antioxidant concentrations, formation of mRNA for procollagen type I and III isoforms, and the proliferation of dermal fibroblasts. The study conducted by Hou and colleagues aimed to explore the potential use of asiaticoside (AE) and madecassoside (MA) as therapeutic compounds for burn recovery and their effects in vivo and in laboratory settings. The study involved 150 male Sprague – Dawley rats with partial thickness skin burns on their backs, totaling 10% of TBSA. The rats were treated with topically applied AE or MA (500 μl) once a day for 14 days. Detailed burn wound evaluations took place on the second, eighth, tenth, and fourteenth time points, with a focus on swelling observed at the surface and base of the wound, exudate, as well as the color and consistency of the tissue surrounding the burn. Measurements of burn wound healing degree were performed using transparent paper on days 2, 8, 10, and 14. Additionally, histopathological examination with hematoxylin – eosin staining was performed to evaluate reformation of the epithelial layer in the burn injury. Overall, the dimensions of the burn wound decreased significantly after day 10. On day 14, the burn wound showed a significant reduction in exudation, swelling, and scab formation. Histopathological assessment revealed increased collagen synthesis, cell proliferation, and re – epithelialization. AE and MA stimulate collagen type I synthesis in dermal fibroblasts by phosphorylating Smad 2 and Smad 3, followed by the complex formation of Smad 3 with Smad 4. Additionally, AE and MA reduce oxidative stress and induce vasodilation. The study also demonstrated that AE and MA had favorable effects on cell growth and replication in animal experiments. It has been reported in prior research that these compounds aid in restoring tissue function by triggering growth factors, including fibroblast growth factors (FGF), endothelial growth factors (EGF), and vascular endothelial growth factor (VEGF) (Hou et al., 2016).
Significant findings were observed in Mayefis' study on the effects of combining Centella asiatica extract and papaya latex extract on burn wound restoration in male white rats. The study involved 35 male white rats with burns, and they were topically treated with test preparations, including single Centella asiatica extract at a 2% concentration and combinations of Centella asiatica extract with papaya latex extract in ratios of 1%:1%, 1.5%:0.5%, and 0.5%:1.5%, with 0.1 grams used topically once a day for ten consecutive days. Burn wound healing was assessed daily by tracking the wound’s diameter and calculating the percentage of healing. The study results showed that increased collagen synthesis and mucopolysaccharide acid contributed to the acceleration of burn wound healing. This occurs by inhibiting the inflammatory phase and aiding in the cleaning of necrotic tissue as well as dissolving dead cells adhering to the skin, which are usually difficult to separate physically. The combination of these factors significantly accelerated the burn wound healing process (Mayefis et al., 2016).
Armadany and his team discovered in their study that applying a combination of ethyl acetate extract from Centella asiatica and virgin coconut oil extract topically twice a day for 21 days on 38 male mice significantly accelerated burn wound healing. Centella asiatica contains alkaloids, flavonoids, tannins (polyphenols), saponins, and terpenoids, which play key roles in this process. Alkaloids, with their astringent and antimicrobial properties, promote wound tissue re-epithelialization, increase the weight of dry granulation tissue, and enhance hydroxyproline enzyme production due to improved collagen maturity. They also prevent cell damage by aiding DNA synthesis, strengthening collagen fibrils, and speeding up tissue regeneration. Flavonoids contribute by promoting wound contraction, reducing the time required for epithelialization, increasing collagen deposition, and enhancing granulation tissue formation. Tannins help by accelerating new tissue growth, acting as an antiseptic to prevent infection, and stopping bleeding by precipitating blood proteins as an astringent. Saponins regulate early collagen development by preventing excess tissue production and encourage new epithelial cell formation, supporting re-epithelialization. Terpenoids exert anti-inflammatory and antibacterial effects, stimulate angiogenesis, and promote the synthesis of collagen type 1, further aiding wound healing. Histological analysis showed flattened fibroblasts—essential cells in the healing process—proliferating and migrating to the wound site to reorganize connective tissue after the injury (Armadany et al., 2023).
The study by Muangman and colleagues was a clinical trial conducted over 21 days using a randomized, double – blind, controlled design. A total of 35 patients with second-degree burns and a TBSA of 20% or greater were involved in the study. The age of participants, both male and female, varied from 18 to 60 years. Patients received burn wound care with polyester gauze coated with a formulation containing 2.5% aloe vera and 5% gotu kola extracts every 3 days until fully healed. The results showed that the treatment group had shorter healing times and hospital stays compared to the control group. Burn area measurements were taken on days 3, 6, 15, 18, and 21. It was observed that smaller burn areas were correlated with higher percentages of epithelialization. This indicates that faster burn healing is associated with higher levels of epithelialization, showing progress in the healing process. Patients in the treatment group exhibited significantly faster healing rates compared to the control group on days 15 and 21. Pain scores were assessed each day using the 11 – point Numeric Rating Scale (NRS – 11). The study results indicated a gradual reduction in pain scores day by day, with significantly lower pain scores in the treatment group on days 14, 16, and 17. A Pseudomonas aeruginosa contamination in the treatment group on day 7 led to the patient’s exclusion from the study. However, no other clinical signs or adverse effects were reported. In light of the study's findings, it is evident that herbal dressings containing 2.5% aloe vera and 5% Centella asiatica can aid in quicker burn wound healing and are linked to reduced hospital stays compared to regular wound dressings (Muangman et al., 2016).
Saeidinia and colleagues demonstrated that 3% Centiderm ointment significantly improved healing, both objectively and subjectively, in under 3 days and enhanced re-epithelialization and complete wound healing more rapidly than silver sulfadiazine (SSD). This was a clinical trial conducted over 25 days using a randomized, double-blind, controlled design. Seventy-five patients with second-degree burns on the limbs and a TBSA of under 10% were recruited to take part, with 60 successfully completing the study. Participants, both male and female, ranged in age from 14 to 60 years. Patients treated their burns once daily at home after receiving instructions on how to use the medication. They also received a medication reminder list that was evaluated each time they attended a follow – up session. Burn evaluations were conducted both objectively and subjectively. Objective evaluations were conducted on days 3, 7, and 14 and included the VSS score (flexibility, vascularity, pigmentation, wound height) and VAS score. The results showed that all objective indices demonstrated significantly better burn healing in the Centiderm group. Subjective evaluations were conducted on days 3, 7, and 14 and included assessments of itching, dryness, and irritation. The results indicated that all subjective indices—itching, dryness, and irritation—showed significantly better burn healing time and effectiveness in the Centiderm group. The Centiderm group showed a significantly quicker re-epithelialization time, with the eschar detaching from the burn wound without leaving a scar. The overall healing process was also faster in this group. There were no signs of adverse effects, such as intense itching, allergic sensitivity, or systemic reactions, during the trial in the Centiderm group (Saeidinia et al., 2017).
Silver sulfadiazine (SSD) cream is a commonly used antimicrobial topical ointment in the treatment of burns. Current burn treatments are primarily aimed at hastening the healing of the skin and preventing infections in the wound. SSD cream offers various advantages, including ease of use and comfort, causing little to no pain upon application, and having low levels of toxicity and sensitivity. Additionally, it possesses strong antibacterial effects, making it a gold standard among antimicrobial topical medications for burn care. As such, it is widely used as a primary medication in burn treatment around the world (Hossain et al., 2020; Saeidinia et al., 2017).
Research highlights that Centella asiatica enhances both objective and subjective healing signs, speeds up re-epithelialization, and supports total healing faster than SSD, while minimizing the risk of infection in patients with partial burns. Additionally, Centella asiatica is more affordable when compared to SSD. Therefore, Centella asiatica can be a viable option for treating partial burns.
Mechanism of burn wound healing by Centella asiatica compounds
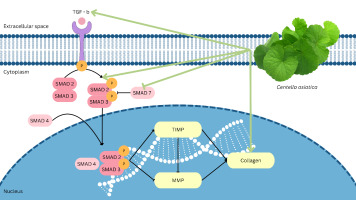
This review incorporates prior research that underscores Centella asiatica's potential in burn wound healing, notably via the TGF-β / Smad signaling mechanism. Typically, the TGF-β / Smad pathway is initiated when TGF-β binds to receptors on the surface of the target cells. Once the receptors bind, they initiate the activation of Smad proteins, which then relocate to the cell nucleus. The Smad complex in the nucleus interacts with other transcription factors to control gene expression related to key cellular functions such as cell growth, specialization, and extracellular matrix development. In the case of burns treated with Centella asiatica, the active compounds, including madecassoside, asiaticoside, madecassic, and asiatic acid, are thought to activate the TGF-β / Smad pathway. Activation of the TGF-β / Smad pathway boosts wound healing by stimulating collagen formation, repairing connective tissue, and regulating inflammatory responses (Bardaa et al., 2016; Hou et al., 2016; Mayefis et al., 2016; Muangman et al., 2016; Saeidinia et al., 2017). Thus, the influence of Centella asiatica on the TGF – β / Smad pathway may be one of the primary processes that underlie the burn wound healing effects seen with this plant, as summarized in Figure 1.
Conclusion
Research involving Centella asiatica has revealed various pharmacological activities, particularly in burn wound healing. The active compounds in this plant (madecassoside, asiaticoside, madecassic, and asiatic acid), have been found to influence the TGF – β / Smad pathway, which is indispensable in the process of burn wound healing. Activation of this pathway increases collagen production, repairs connective tissue, and regulates inflammatory responses, all of which contribute to burn wound healing. Clinical research has also demonstrated the effectiveness of herbal dressings based on Centella asiatica in accelerating burn wound healing and reducing hospital stay duration. Therefore, Centella asiatica offers potential as a valuable burn wound healing agent, particularly through its influence on the TGF – β / Smad pathway. Additional in vitro and in vivo studies are required to assess the potential of Centella asiatica in burn wound healing.
Conflicts of Interest
The authors declare that there is no conflict of interest related to the publication of this review paper.
Funding
This article received funding support for the publication fee from Universitas Kristen Maranatha.
Author Contributions
EHDS, JWG, and TLW were responsible for the conception and design of the study, providing the conceptual framework and overall study design. Data collection and acquisition were led by EHDS, with contributions from TLW. EDHS, JWG, and TLW performed the data analysis and contributed to its interpretation, ensuring the results were accurately understood and contextualized. The manuscript was initially drafted by EHDS, with JWG and TLW providing critical revisions to enhance the intellectual content and overall quality of the work.